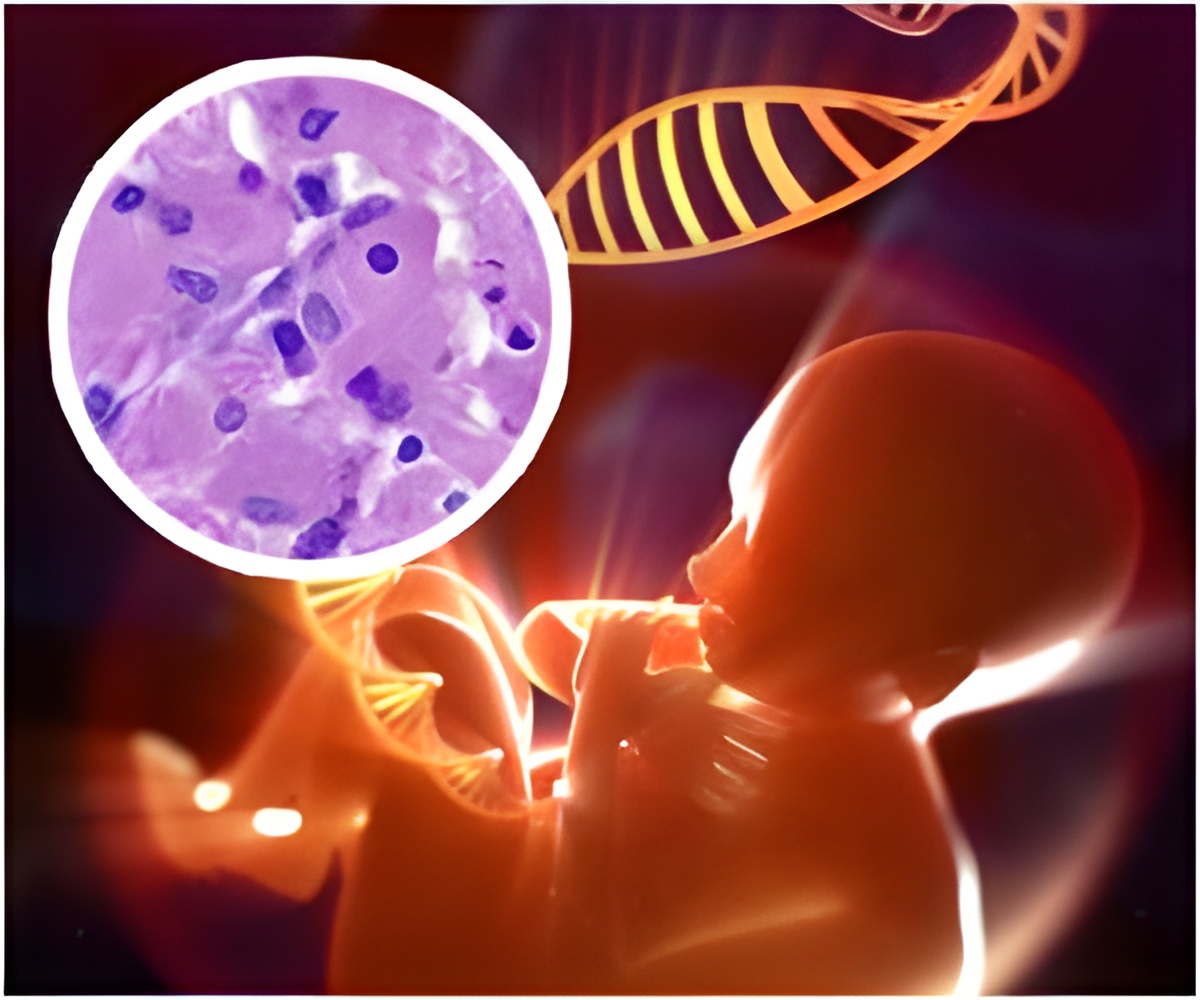
"In the past decade, there has been a significant increase in opioid use during pregnancy, estimated to affect 5.6 per 1,000 births," according to background information in the article. Neonatal abstinence syndrome is a disorder composed of a constellation of signs and symptoms involving dysfunction of the nervous system, gastrointestinal tract, and respiratory system because of in utero drug exposure or iatrogenic (due to therapy) withdrawal after maternal use of drugs for pain control during pregnancy. "The incidence of NAS has tripled in the past decade, affecting 60 percent to 80 percent of infants born to mothers receiving methadone or buprenorphine. Although clinical factors, including maternal smoking, psychiatric medications, and breastfeeding, can affect the incidence and severity of NAS, to our knowledge contributing genetic factors influencing NAS have not been pre¬viously identified."
Variations in the genes OPRM1, ABCB1, and COMT are associated with risk for opioid addiction in adults. Dr. Davis and colleagues conducted a study to determine whether genomic variations in these genes are associated with length of hospital stay (LOS) and the need for treatment of NAS. The study was conducted at 5 tertiary care centers and community hospitals in Massachusetts and Maine between July 2011 and July 2012. DNA samples were genotyped for single-nucleotide polymorphisms (SNPs), and NAS outcomes were correlated with genotype.
Eighty-six of 140 eligible mother-infant dyads (pairs) were enrolled. Infants were eligible if they were 36 weeks' gestational age or older and exposed to methadone or buprenorphine in utero. Eighty-one (94 percent) of the mothers were receiving opioid substitution therapy from the first trimester, with 17 (20 percent) relapsing into illicit drug use during the third trimester. Average LOS for all infants was 22.3 days; for treated infants, 31.6 days. Fifty-six (65 percent) of all infants were treated for NAS.
The researchers found that infants with the OPRM1 118A>G AG/GG genotype had shortened length of stay (-8.5 days [calculated with linear regression models]) and were less likely to receive any treatment than infants with the AA genotype (48 percent vs. 72 percent). "The COMT 158A>G AG/GG genotype was associated with shortened length of stay (-10.8 days) and less treatment with 2 or more medications (18 percent vs. 56 percent) than the AA genotype. Associations with the ABCB1 SNPs were not significant."
"To our knowledge, this is the first study to examine the association of genomics with opioid withdrawal in infants and may provide insight into the mechanisms underlying NAS. There is a need for replication of these results before more definitive conclusions can be made of the association between the OPRM1 and COMT variants and NAS," the authors conclude.
Advertisement