Antibiotic resistance threatens health and lives.
Since 2005, MRSA have killed over 18,000 people a year in the United States alone.
To make matters worse, in 2002 a new MRSA with resistance to even the last-line drug vancomycin (VRSA) appeared.
Scientists at the Centers for Disease Control, Harvard University and elsewhere have been working to determine the origin of these VRSA, to understand why they have turned up, and to understand the risk of spread.
Most VRSA occurred in foot and limb infections of diabetics who are often in and out of health care facilities. Each of these infections is believed to have had multiple bacteria, an MRSA plus a vancomycin resistant bacterium called Enterococcus (or VRE). VRE has caused vancomycin resistant hospital-acquired infections since the 1980s.
Advertisement
They have also demonstrated that resistance arose independently in each strain after it acquired a specific bit of genetic material called transposon Tn1546.
Advertisement
The Harvard-wide Antibiotic Resistance Program is using this information to develop new ways to prevent and treat infection by MRSA, VRSA and VRE.
The team identified several new compounds that stop MRSA by hitting new targets, and is currently subjecting these to further tests.
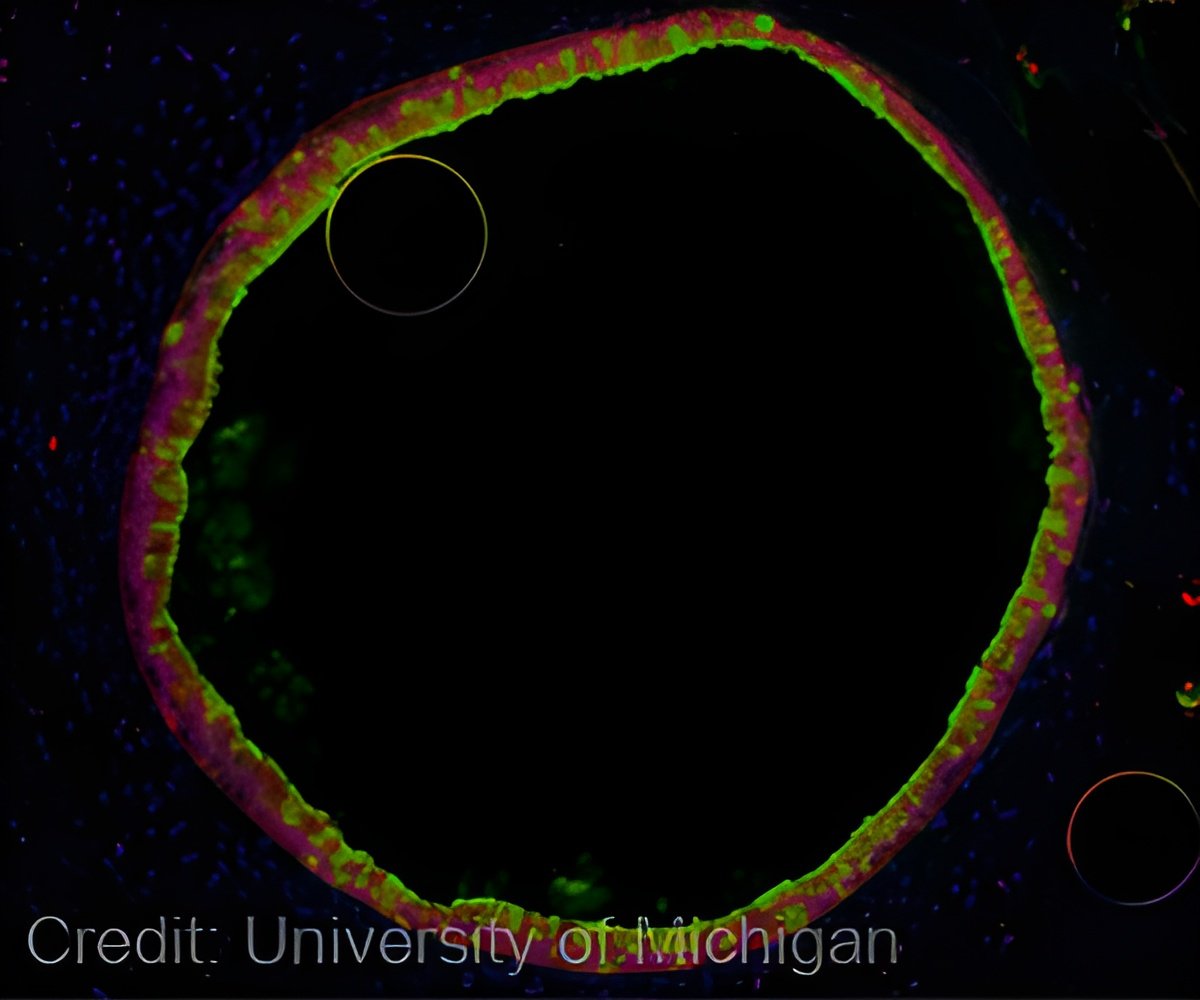
To sequence the genomes, researchers from the National Institutes of Health (NIH)-funded Harvard-wide Antibiotic Resistance Program, headquartered at the Massachusetts Eye and Ear in Boston, assembled an elite international team.
Headed by Harvard professor Michael Gilmore, Ph.D., and his associate Veronica Kos, Ph.D., both based at Mass. Eye and Ear, the team included bioinformatics and genomics experts from the Broad Institute of MIT and Harvard, the Institute for Genome Sciences of the University of Maryland, the University of Rochester, and the Wellcome Trust Sanger Center in the UK.
They identified features in the genomes that appear to have made it easier for certain MRSA to acquire resistances in mixed infection.
"The genome sequence gave us unprecedented insight into what makes these highly resistant bacteria tick. Several things were remarkable," said Gilmore.
"Vancomycin resistance repeatedly went into just one tribe of MRSA, so the question became 'what makes that group special-why did they start getting vancomycin resistance?'"
"What we found was that this group of MRSA has properties that appear to make it more social, so they can live with other bacteria like Enterococcus. This would allow those MRSA to more easily pick up new resistances," said Kos.
"The good news is that some of these properties weaken the strain's ability to colonize, and may be limiting their spread," he added.
Their findings are reported in the May 22 issue of the journal mBio, the American Society of Microbiology's first broad-scope, online-only, open access journal.
Source-ANI