Duke University Medical Center scientists hope to improve scientific understanding of lung disease, having found that a single lung cell can become one of two very different types of airway cells.
The researchers shown this using both animal and human cells in their experiments.They used a single "basal" cell-a small, squat stem cell that divides to replenish the lung lining layer-to create 3-D hollow spheres that were lined inside with both ciliary and secretory cells.
Dr. Brigid Hogan, chair of the Duke Department of Cell Biology, says that this 3-D model can be used to study dynamic processes underlying lung diseases, including cancer.
"Now that we have this 3-D model and information about the gene expression 'signature' of basal cells, we are in a strong position to see what happens when lung-cell behavior goes awry.
We might, for example, be able to activate an oncogene (a cancer-causing gene) or other factors to see how lung cancer might develop in the airways. Amazingly, almost nothing is known about lung basal cells, which are so important to health and make up nearly a third of the cells in the human airways," Hogan said.
Basal stem cells generally maintain the airways by turning over slowly into new ciliated cells and secretory cells.
Advertisement
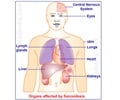
Both types of cells are neatly arranged in equal proportions in healthy lung airways. But when lungs are affected by diseases like cancer, chemical damage, cystic fibrosis or asthma, the balance of these cells can be thrown off.
Advertisement
"We put a lot of effort into developing this model, so that we and other groups can test the ability of individual airway progenitor cells to divide and differentiate under defined conditions.
Now we can change the culture conditions to investigate mechanisms that underlie pathological conditions, including chronic asthma and cancer," said lead author Dr. Jason Rock, a postdoctoral associate in the Duke Department of Cell Biology.
The researchers have also found that one gene expressed in the basal cells encodes a surface receptor, also found on human lung basal cells.
"This meant we were able to use a labeled antibody against this receptor to efficiently extract human lung basal cells to create the human bronchospheres for study," Hogan said.
A research article describing the study has been published in PNAS Early Edition.
Source-ANI