Bisphosphonates are drugs that help prevent or slow down bone thinning (osteoporosis). They can help to treat some types of cancer that cause bone damage.
‘The Food and Drug Administration is now recommending patients use bisphosphonates for three to five years, followed by reassessment of their risk.’





But there is a caveat: Prolonged use of these drugs can alter the composition of bone, making it more brittle and more susceptible to a rare but serious form of fracture. And a group led by Eve Donnelly, assistant professor of materials science and engineering at Cornell University, has put forth a couple of possible explanations for this phenomenon. Her group - in collaboration with researchers from Weill Cornell Medicine and the Hospital for Special Surgery in New York, among others - detail their findings in "Atypical Fracture with Long-Term Bisphosphonate Therapy is Associated with Altered Cortical Composition and Reduced Fracture Resistance," published July 31, 2017, in the Proceedings of the National Academy of Sciences.
Modern medicine and attention to healthier lifestyles has contributed to people living into their 80s, 90s and beyond. Some estimates say that by 2050, the number of U.S. residents age 65 and older will be near 84 million, nearly double the 2012 total.
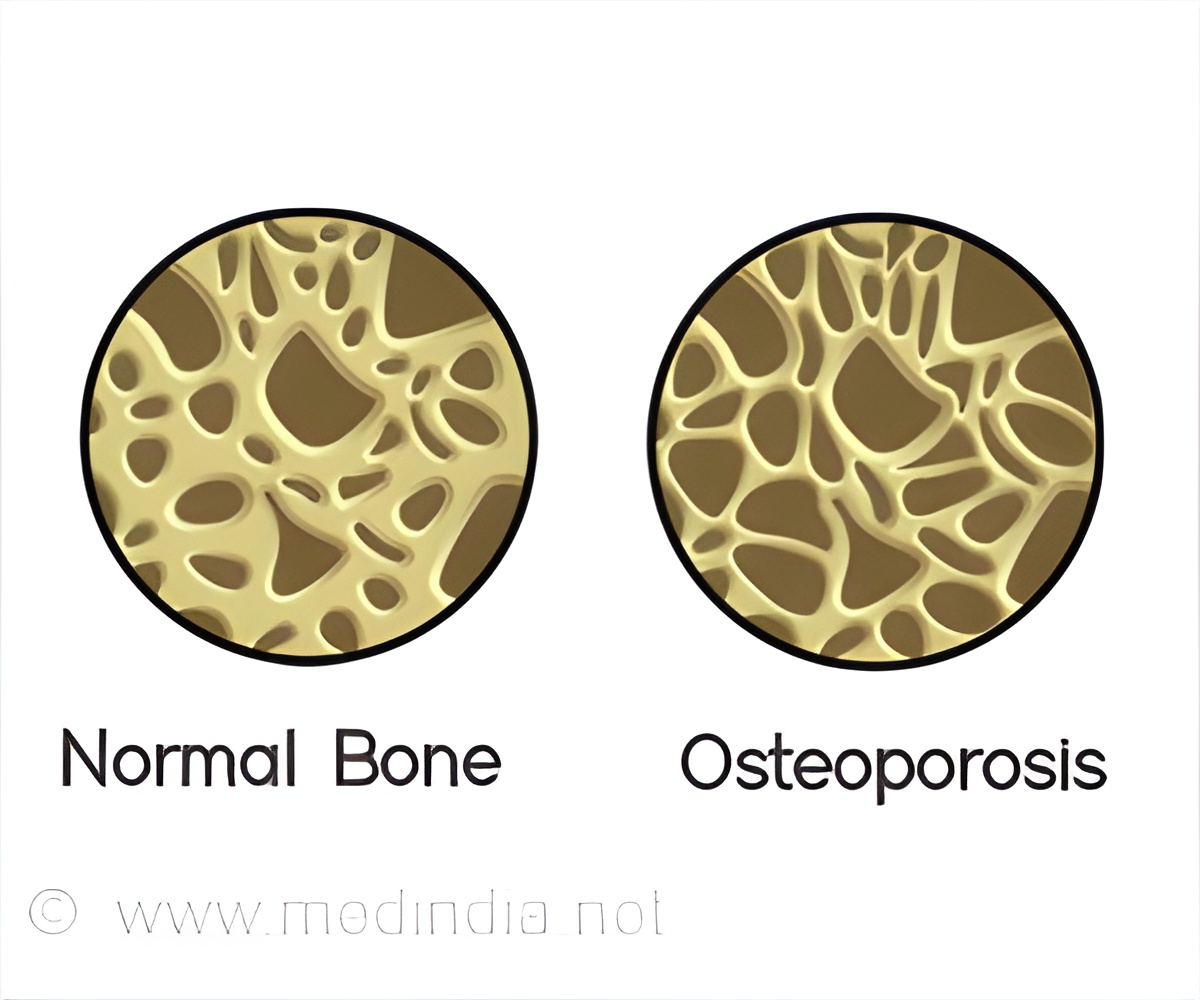
But that has also made more people - especially postmenopausal women - vulnerable to conditions such as osteoporosis, a loss of bone tissue due in part to hormonal changes.
"Because of the changing demographics of our country," Donnelly said, "the Surgeon General's office estimates that by the year 2020, half of our population over age 50 will either have or be at risk for fractures from osteoporosis."
Advertisement
For this study, the team examined biopsies of cortical bone - the outer layer - from the shaft of the femur obtained from postmenopausal women during fracture repair surgery. Analysis of bone samples was conducted at the Cornell Center for Materials Research and with collaborating labs at University of California Berkeley and University Medical Center Hamburg-Eppendorf.
Advertisement
The testing pointed to a couple of contributing factors: Bisphosphonate-treated women with AFF had bone that was harder and more mineralized than bisphosphonate-treated women with typical osteoporotic fractures. Donnelly said this is due to bisphosphonates' main function: slowing the resorption (shedding) of old bone, which is typically followed by remodeling, the growth of new bone. In healthy adults, cortical bone is constantly being resurfaced, such that the entire adult skeleton is overhauled every 10 years or so.
But that resurfacing process begins with resorption, and if resorption is slowed by bisphosphonates, the remodeling process is also affected. The result: The existing bone ages and gets brittle over time.
"It's kind of a double-edged sword," Donnelly said. "It's extremely good to prevent bone loss, but the drugs will also slow this natural process, which allows turnover."
The other unforeseen side effect to long-term bisphosphonate use involves crack-deflection - the resurfaced bone's ability to stop a microscopic crack from propagating, which can lead to a break. New layers of bone can act as a "firewall" of sorts, stopping a crack from spreading, but mineralized, older bone loses that function.
"Bone usually has natural variability in mineralization within the tissue, which may help to deflect cracks," Donnelly said. "As you increase the mineralization, you may tend to lose that natural variation."
The Food and Drug Administration is now recommending patients use bisphosphonates for three to five years, followed by reassessment of their risk. Donnelly makes it clear that her study is not proposing doing away with bisphosphonate treatment. Studies have estimated the risk of AFF among bisphosphonate users at between one and 10 in 10,000, and have shown the benefit of bisphosphonates continues to far outweigh the risk of AFFs.
One study, published in 2011 on pubmed.gov, estimated that for each reduction of 100 typical hip fractures associated with bisphosphonate use, there was an increase of one AFF.
"That's one of the cautions I'd like to impart," Donnelly said. "What we have observed is really the result of long-term treatment, well beyond what the FDA is recommending for these drugs now. Our work explains some of the underlying mechanisms of AFFs and can inform the refinement of dosing schedules for patients at risk of fragility fractures."
Source-Eurekalert















