Elena Goncharova, PhD, research assistant professor of Medicine, and Vera Krymskaya, PhD, associate professor of Medicine, Pulmonary, Allergy, and Critical Care Division at Penn, led the study. The team collected TSC2-mutant cells from spontaneous kidney tumors formed in mice. They then "sensitized" those cells by growing them into tumors in immunocompromised mice, excising those tumors, and reinjecting their cells into the tail veins of another set of immunocompromised mice.
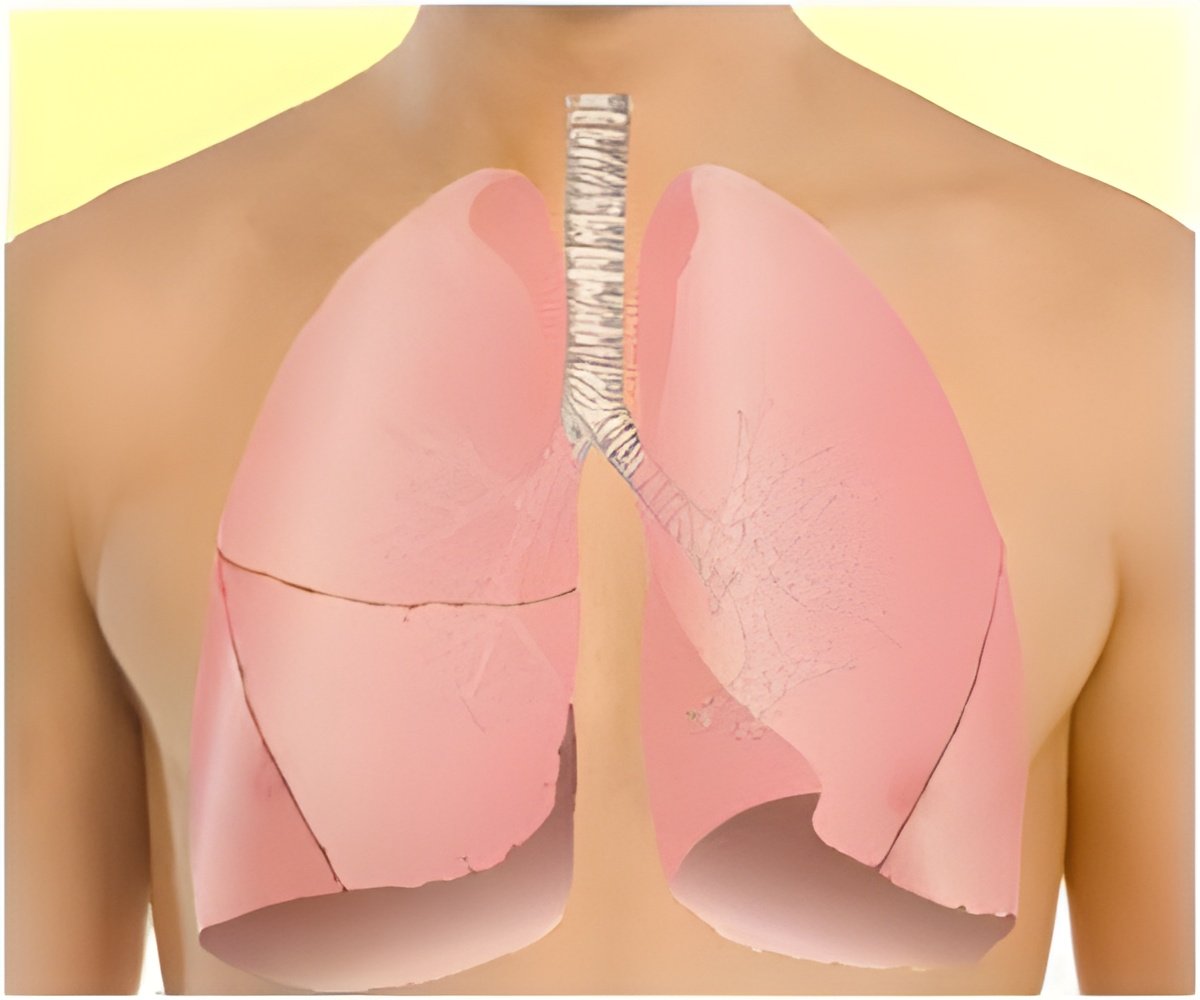
Unlike non-sensitized TSC2-deficient cells, the sensitized cells produced multiple lung nodules comprised of smooth muscle-like cells, as in the human disease, as well as destruction of lung tissue and lymphangiogenesis. These nodules also exhibited enhanced activity of an enzyme called matrix metalloproteinase and the loss of elastin, suggesting a potential mechanism for causing that tissue damage. The study also demonstrated for the first time that destruction of lung tissue in LAM is caused by TSC2 deficiency in lung lesions.
TSC1 and TSC2 regulate the mTOR (mammalian target of rapamycin) pathway. As a result, the antibiotic rapamycin is already used therapeutically for pulmonary LAM. But, says Goncharova, the drug appears only to halt cell growth, not induce cell death. When rapamycin is removed, disease progresses. "That showed us that something else was needed to fully treat the disease," she says.
As it turns out, that something else could be a statin.
Statins are well known cholesterol-controlling medications. But they also can inhibit signaling proteins called GTPases, inducing cell death. An earlier study using rapamycin and simvastatin demonstrated that the combination could prevent tumor reoccurrence in a mouse model in which TSC2-mutant tumors were not grown in the lungs, but in the flanks of the animal.
Advertisement
But perhaps more importantly, from a clinical point-of-view, application of the drugs after development of lung nodules and tissue damage could actually reverse tissue damage.
Advertisement
As in the earlier study, rapamycin in this study appears to be cytostatic – it halts cell growth; simvastatin induces cell death, and both drugs block matrix metalloproteinases as well. Both drugs are FDA-approved and commercially available.
But before pulmonary LAM patients call their physicians for a prescription, Goncharova stresses that the results were in mice, not humans. Clinical trials are required to test the efficacy of this drug combination in patients. To date, no such trials have been initiated.
"I hope it will be done in the near future," she says.
Source-Eurekalert