‘Paroxetine could be the first antidepressant drug to improve key symptoms of cognitive impairment in people with HIV.’
Tweet it Now
The researchers note that many patients with HIV-associated neurocognitive disorders may already be benefiting cognitively by taking SSRIs in the dosages used in their study to treat depression, but the new study lends more rigorous scientific support to the drug's value. The Johns Hopkins researchers are expected to present their findings Feb. 25 at the Conference on Retroviruses and Opportunistic Infections in Boston.
"Over a period of 20 years and after 10 clinical trials, this is the first time we've been able to clearly demonstrate benefit in a summary measure of cognitive performance for patients with HIV-associated neurocognitive disorders," says lead author Ned Sacktor, professor of neurology at the Johns Hopkins University School of Medicine.
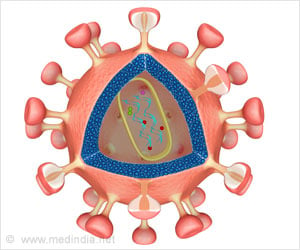
HIV-associated neurocognitive disorders occur when infection with the virus that causes AIDS triggers nerve-damaging inflammation in the brain, leading to problems with learning, memory, decision-making and motor coordination. Up to 50 percent of people with HIV taking a cocktail of antiretroviral drugs are estimated to suffer from cognitive impairment, the researchers say.
In a search for a drug to safely blunt inflammation and reverse impairment, the investigators chose to test two drugs that looked promising based on earlier data published in 2014 by co-author Joseph Steiner, an adjunct associate professor of neurology.
Advertisement
"There is a huge advantage to incorporating FDA-approved drugs into a clinical trial rather than developing whole new ones," says senior author Justin McArthurprofessor and director of the Department of Neurology. "It's quicker, cheaper and very unlikely that there will be any surprises or any untoward side effects because the drug has been given to tens of thousands of people already."
Advertisement
The team used eight neuropsychological tests to measure and evaluate psychomotor and motor speed performance and decision-making. The NPZ8 score, as it's called, comes from averaging the eight test results and evaluating this number using a statistical test that compares HIV positive patient test scores to HIV negative scores. The numerical score represents the standard deviation from the mean. Patients given paroxetine alone or in combination with fluconazole improved their NPZ8 test scores by an average of 0.15. Those not taking paroxetine showed a deterioration of their score by -0.33 on this same measure of cognitive performance.
At the start of the trial and after 24 weeks of drug treatment, patients were also assessed on reaction times using the California Computerized Assessment Package (CalCAP) test, which asks participants to complete tasks like pressing a button when they see a number on the screen.
Patients taking paroxetine improved test scores on a subset of the CalCAP test by a 0.5 increase over the baseline measurement, but those not taking paroxetine showed essentially no improvement, with only a 0.06 change in score.
To learn if either or none of the drug treatments reduced levels of inflammatory proteins in the patients -- a measure of inflammation -- the physicians took blood samples from the patients at the start of the study and at 24 weeks after drug treatment. They measured the level of CD163, which is known to be higher than average in patients with HIV-associated neurocognitive disorders and an indicator of inflammation. Before treatment, patients with HIV had an average of 802 nanograms per milliliter of CD163 protein in the blood, but after treatment with paroxetine, the average level dropped to 738 nanograms per milliliter. Patients not given paroxetine saw their CD163 levels rise by an average of almost 400 nanograms per milliliter over the 24 weeks.
"By reducing inflammation, we hoped to have the added benefit of improving cognition, and our results show that to be the case," says Sacktor.
Because the team found no cognitive improvements with fluconazole alone, Sacktor says his work may now focus on larger studies using paroxetine alone.
Paroxetine treatment typically costs less than $15 a month. Some study participants reported side effects typical of SSRIs after taking paroxetine, including sexual dysfunction (three patients), headache (two patients), insomnia (two patients) or vivid dreams (two patients). SSRI therapies for depression or anxiety don't always work for everyone, and people do discontinue using these drugs because of unwanted side effects. Researchers do not yet know the precise mechanism by which an SSRI may improve cognitive impairment.
Source-Eurekalert