- Scientists have suggested the re-classification of diabetes based on several variables.
- The re-classification could be used to develop a more personalized approach to the treatment of diabetes, which could in turn improve glycemic control and reduce the chances of complications.
- The presence or absence of glutamate decarboxylase antibodies; these antibodies are present in patients with type 1 diabetes patients
- The age of the individual at the time of diagnosis of diabetes
- The body mass index (BMI)
- The HbA1c measurement. A level of less than 6.0% is considered normal
- The homoeostatic model assessment 2 estimates of β-cell function. The β-cells are the cells of the pancreas that secrete insulin
- The presence or absence of insulin resistance based on the concentration of C-peptide
Cluster 1 included patients with severe autoimmune diabetes (SAID). The individuals were insulin deficient, tested positive for GAD antibodies, had poor metabolic control, and were young and lean with a relatively low BMI. Cluster 1 corresponds to the current type 1 diabetes and latent autoimmune diabetes in adults (LADA).
Cluster 2 included individuals with severe insulin-deficient diabetes (SIDD); GADA antibodies were absent in these individuals. This group was at the highest risk of diabetic retinopathy, a form of eye damage caused by diabetes that can result in blindness.
Clusters 1 and 2 had the highest HbA1c levels, which indicated poor diabetes control. Patients in these clusters were also more likely to suffer from ketoacidosis at the time of diagnosis of the diabetes. Ketoacidosis is a life-threatening complication of diabetes that results in high blood ketone levels. It has to be treated on an emergency basis.
Cluster 3 included individuals with severe insulin resistance (severe-insulin resistant diabetes (SIRD)). They had a high body mass index, and were at the highest risk for diabetic kidney disease.
Cluster 5, referred to as mild age-related diabetes (MARD), included individuals with diabetes that appeared at an older age and was associated with modest metabolic alterations.
The variety of medications available for the treatment of diabetes has increased in the past few years. An appropriate use of these medications in different populations of diabetes patients could result in better outcomes and reduced complications.
Type 1 and Type 2 Diabetes
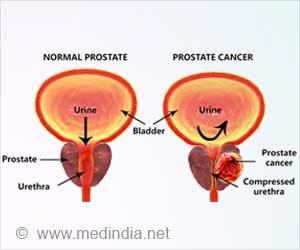
Diabetes is a condition where the blood levels of glucose rise and remain above the normal. Persistent high blood glucose levels are associated with several complications. Type 1 diabetes is a form of diabetes where the pancreas fail to produce adequate insulin due to an immunological disorder; the patients develop antibodies against the pancreatic cells that secrete insulin. The condition often affects younger individuals, and is therefore referred to juvenile onset diabetes. The affected individuals are usually lean and require life-long treatment with insulin. Type 2 diabetes usually affects adults, who can be treated with oral medications, until they progress to a point where they require insulin. It occurs due to reduced sensitivity of tissues to insulin. The affected individuals often tend to be overweight. Other lesser forms of diabetes include latent autoimmune diabetes in adults (LADA), maturity-onset diabetes in the young (MODY), and secondary diabetes.References:
- Emma Ahlqvist et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. The Lancet Diabetes & Endocrinology.
- Rob Sladek. The many faces of diabetes: addressing heterogeneity of a complex disease. The Lancet Diabetes & Endocrinology.