Researchers at the University of Pittsburgh Schools of the Health Sciences studying links between an early sign of heart disease called coronary artery calcification and body fat have found that, paradoxically, more fat may have some advantages, at least for people – particularly women – who have type 1 diabetes.
Cardiovascular complications, including heart disease, are a leading cause of death for people with diabetes, who tend to suffer cardiovascular disease decades earlier than non-diabetics.“Gaining weight may reflect good or better treatment with insulin therapy, which may partly explain why participants who gained weight over time had lower mortality rates,” said Trevor Orchard, M.D., professor of epidemiology at the University of Pittsburgh Graduate School of Public Health (GSPH).
For this particular report, Dr. Orchard and his colleagues focused on 315 patients with type 1 diabetes participating in the Pittsburgh Epidemiology of Diabetes Complications Study, an 18-year prospective study of childhood onset type 1 diabetes, which began in 1986. As part of the study, the patients recently received a special computed tomography scan (CT) to assess coronary artery calcification.
Omega-3 fatty acids create chemical compounds known as bioactive mediators, which protect against the growth of abnormal blood vessels, a condition that characterizes some forms of retinopathy. In part, this occurs because these mediators suppress a type of inflammatory protein called tumor necrosis factor alpha (TNF-alpha). TNF-alpha is found in one type of cell, called microglia, that can be closely associated with retinal blood vessels.
“The retina has one of the highest concentrations of omega-3 fatty acids in the body,” said lead author and NEI fellowship recipient Kip M. Connor, Ph.D., a postdoctoral research fellow at Children’s Hospital Boston. “Given this, it is remarkable that with only a two percent change in dietary omega-3 intake, we observed an approximate 40-50 percent decrease in retinopathy severity.”
“Our findings represent new evidence suggesting the possibility that omega-3 fatty acids act as protective factors in diseases that affect retinal blood vessels,” said John Paul SanGiovanni, Sc.D., NEI staff scientist and the other lead author of the study. “This is a major conceptual advance in the effort to identify modifiable factors that may influence inflammatory processes implicated in the development of common sight-threatening retinal diseases.”
Advertisement
"The purpose of our study was to discover and describe the scientific basis for any possible protective role of omega-3 fatty acids against retinopathy,” said Lois E. H. Smith, M.D., Ph.D., senior investigator of the study and associate professor of ophthalmology at Children’s Hospital Boston, an affiliate of Harvard Medical School.
Advertisement
This changing of lipids by dietary means may also translate to AMD and diabetic retinopathy. If clinical trials find that supplementing with omega-3 fatty acids is as effective in protecting humans against retinal disease as demonstrated by the findings of this study, this cost effective intervention could benefit millions of people."
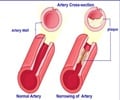
The participants’ mean age was 42, and mean duration of diabetes was 34 years. In addition to the CT scan, patients were evaluated for fat underneath the skin and in the abdominal region, body mass index (BMI) and waist circumference. Although investigators noted a positive association for all measures of fatness and having any coronary artery calcification, in the two-thirds of patients who had calcification, the relationship reversed so that people with more fat had less severe calcification. This association also varied by gender. Women with less fat under the skin had more evidence of coronary artery calcification than those with more fat. Thinner men also had more evidence of coronary artery calcification than men with a higher BMI. “What it comes down to is a kind of double-edged relationship,” said Baqiyyah Conway, M.P.H., lead author of the abstract, adding that these associations of less severe artery calcification with greater fat persisted even when controlling for standard cardiovascular disease risk factors such as increased levels of LDL, or bad cholesterol, triglycerides, high blood pressure and lower levels of HDL, or good cholesterol. Controlling for kidney disease, another common complication of diabetes, weakened the association in men but not in women. “This is not a firm recommendation to people with type 1 diabetes to put on weight, but it does raise the possibility that weight recommendations in type 1 diabetes may be somewhat different than those for the general population, and emphasizes the complex relationship between body fat and cardiovascular risk in diabetes,” said Dr. Orchard, who also is professor of medicine and pediatrics at the University of Pittsburgh School of Medicine.
Source-Eurekalert
GPL/M