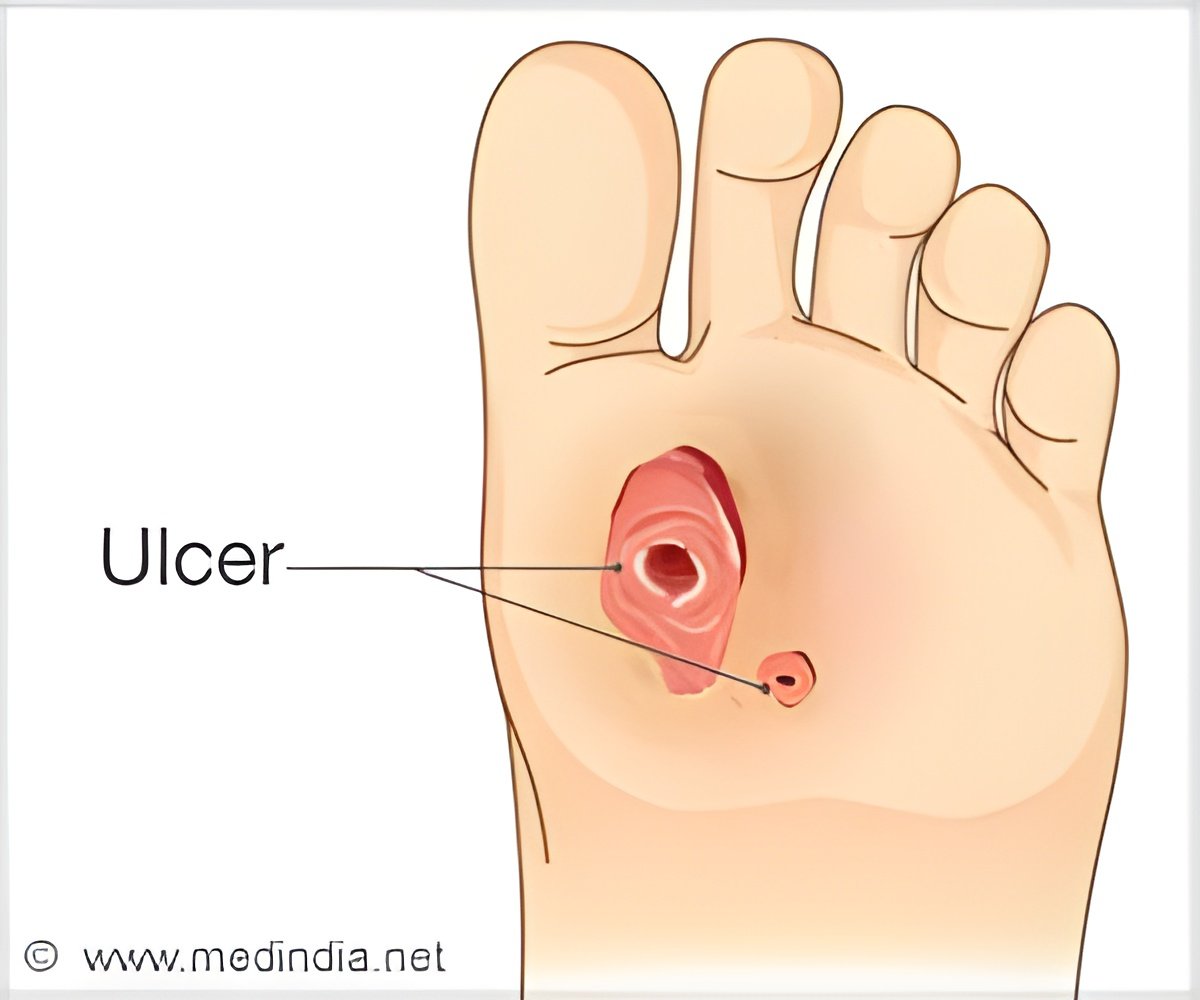
‘Chronic wounds are a primary complication of diabetes. Monitoring the bacterial populations of diabetic foot ulcers may help doctors determine the best way to treat them.’
Read More..Tweet it Now
About 10 percent of Americans have been diagnosed with diabetes, and one-quarter of these patients will develop a wound that does not heal. In the worst case outcome, which occurs in up to 25 percent of these wound-developing patients, the wounds will require an amputation. Many patients who develop these ulcers may not notice the initial signs since the high blood glucose of diabetes can lead to a lack of feeling and deformation of the feet. Read More..
As a result, patients with diabetes commonly develop foot ulcers that may go unnoticed over time. Current treatments are insufficient, meaning patients can live with these wounds for months or even years without healing. The mortality rate associated with diabetic foot ulcers is equivalent to that of breast cancer and prostate cancer combined - higher than 70 percent when they lead to amputation.
"While wounds don't receive the attention of other diseases, they're incredibly common, and our study increases our understanding of how microbes impair or promote healing," said the study's senior author Elizabeth Grice, Ph.D., an associate professor of Dermatology. The lead author, Lindsay Kalan, Ph.D., now an assistant professor of Medical Microbiology and Immunology at the University of Wisconsin School of Medicine and Public Health, began this work as a post-doctoral researcher in Grice's lab.
Previous studies have used lower resolution techniques to catalog the microbes that reside in chronic wounds. This study built on that research by using higher resolution DNA sequencing to identify specific species and subspecies and how they are related to patient outcomes. Researchers collected samples from 46 patient ulcers every two weeks for six months, or until the wound healed or was amputated.
S. aureus, a common and difficult-to-treat pathogen, was found in the majority of wounds, but researchers note the presence of the bacteria itself did not predict whether or not a wound would heal. However, the high-resolution DNA sequencing showed certain strains of S. aureus were only in the wounds that did not heal over the course of the study. Further testing revealed that the "non-healing" strain was better equipped to cause tissue damage and evade antibiotic treatments. Researchers further validated their findings in mice.
Advertisement
"It is possible there are bacteria that actually benefit the wound, and we can use what we learned in this study to develop new treatment strategies for non-healing wounds," Grice said. "We hope this research will eventually help identify patients at risk for bad outcomes and lead to treatment innovations that these patients desperately need."
Advertisement















