Some epidemiologists, physicians and scientists have begun to "shift attention away from technological fixes," such as vaccines, to prevent HIV transmission toward "proven, lower-tech strategies," after Merck's experimental vaccine trial was halted in September, the Washington Post reports.
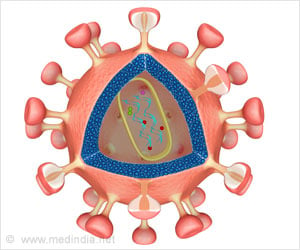
Merck in September announced that it had ended its Phase II trial, which began in late 2004 and involved 3,000 HIV-negative volunteers, after its experimental vaccine failed to prevent HIV infection in participants or prove effective in delaying the progression of the virus to AIDS. The trial was stopped by the Data and Safety Monitoring Board, an independent overseer. Some researchers have theorized that because HIV-positive people who have stronger CD4+ T-cell responses tend to fight the virus better, a vaccine that simulated a T-cell response might be able to control HIV/AIDS. The Merck vaccine was made from a weakened version of a common cold virus that served as a mode for providing three synthetically produced genes from HIV, known as gag, pol and nef.According to the Post, there are "few promising vaccine candidates," and "pressure is building" from some experts to focus on other prevention strategies, such as male circumcision, promoting sexual monogamy and providing contraception to HIV-positive women. The "science behind several existing but lower-tech approaches has grown stronger" as efforts to develop a vaccine for HIV have "faltered," the Post reports. Male circumcision provides some level of "lifelong protection," and a reduction in the number of people who have multiple sex partners led to declines in HIV cases in Kenya and Uganda, the Post reports. Access to contraception also can prevent HIV-positive women from conceiving and giving birth to infants who might contract the virus. Although antiretroviral drugs can prevent mother-to-child HIV transmission, the drugs are available to only one in 10 African women who need them, according to the Post.
In addition, prevention strategies that work during trials often do not work in the "context of actual sexual behavior," the Post reports. Health workers routinely use antiretrovirals when stuck by HIV-infected needles; however, the difference in HIV incidence among women in West Africa who were asked to take antiretrovirals as part of a study was "so small that scientists could not determine whether the medicine worked," according to the Post. Although condoms can prevent HIV transmission, they are not used often enough to reverse the spread of HIV in sub-Saharan Africa, the Post reports. The "unpredictable nature of human behavior helps explain the enduring allure of a vaccine," according to the Post.
One challenge in implementing lower-tech strategies is that they "do not attract the money or attention" that vaccines or microbicides do, the Post reports. A recent United Nations report that called for increased spending on HIV/AIDS recommended about 1% of total spending be allocated for programs that promote male circumcision or encourage changes in sexual behavior. The report also did not allocate funds to increase contraceptive access.
According to Malcolm Potts, a professor at the University of California- Berkeley, it is "criminal not to put money into the things that work, and the things that work are relatively inexpensive." Glenda Gray, the lead South African researcher on the Merck trial, added, "Without a biomedical instrument to prevent HIV, basically the world will never be able to control HIV because people will never stop having sex"
Source-Kaiser Family Foundation
SRM/V