What exactly is Aquatherapy? How does it work? Who is it suitable for? Medindia got the answers from Dr. Jan Prins who is a professor at the University of Hawaii and the director of the Aquatics Research Laboratory. He has now established an aquatic physical therapy clinic in Colombo, Sri Lanka, bringing the program to the country of his birth.
1. Can you tell us what medical conditions can be effectively treated by Aquatherapy? Is there any one condition it is particularly useful for?Aquatherapy is effective in the treatment of a large variety of conditions. I do not think there is any single condition that it is more effective than any other. Clearly, conditions that are exacerbated by gravity, i.e. weight-bearing, respond well in the water.
1. Orthopedic conditions associated with the major joints: Neck, back, shoulder, hip, and knee injuries
2. Recovery from work injuries and auto accidents
3. Hip & knee replacement
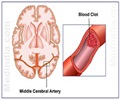
4. Recovery from CVA’s (stroke) and neurological injuries which includes “balance training” for fall prevention.
5. Rheumatological conditions - Arthritis, Fibromyalgia
6. Diabetes – exercising with a reduction in joint trauma.
7. Athletic injuries.
8. Osteoporosis.
9. Conditions exacerbated by changes in body alignment during pregnancy.
10. Injuries that are either recent, or old, but still cause pain and discomfort.
2. What Makes Aquatic Therapy Work?
Two important physical properties of water, buoyancy and viscosity, are key elements in designing effective aquatic exercises.
The advantage derived from buoyancy is direct; when a person enters the water there is an immediate reduction in the effects of gravity on the body. The buoyant force of water decreases the effective weight of an individual in proportion to the degree of immersion. The ability to control joint compression forces by varying degrees of immersion is of primary benefit in the design and prescription of conditioning and therapeutic exercises. By monitoring the depths at which functional movements such as walking and stepping are performed, the effect of gravity can be re-introduced and, consequently, gradual strengthening is promoted.

The viscosity of the water has an indirect advantage; when moving through the water, resistance is felt. The degree of effort is determined by the size of the moving body or limb, coupled with the velocity of the movement. Although traditional modes of strength training are used successfully on land, there are primary advantages for using water resistance to promote strengthening. Water acts as a variable accommodating resistance. The advantage of an accommodating resistance is that it matches the applied force or effort. Because the resistance of the water equals the force exerted, the probability of exceeding tissue tolerances is reduced and the likelihood of exacerbation when building strength after injury or re-injury is dramatically reduced.
3. What are the kinds of results we can expect from Aquatherapy? Can you tell us if aqua-therapy can help people with backache and for treating other conditions associated with the spine?
Axial loading on the spine and weight-bearing joints, particularly the hip, knee, and ankle, is reduced with increasing depths of immersion. When standing in chest-deep water the weight-bearing load is approximately 40% of the total body weight. When stepping up onto a submerged step in the water, the body rises to waist-depth, increasing the gravitational load to approximately 60% of body weight. When floating in the prone, supine, or vertical positions, the effects of gravity are, for all practical purposes, eliminated.
Because axial and compressive forces are reduced in the water, a case can be made for early prescription of aquatic therapy. When it is premature to resume full weight-bearing activities but important to beginning closed kinetic chain exercises, exercising in the water at graduated depths is ideal. These patients can later transition to land-based physical therapy to continue their prescribed rehabilitation program.
4. Can you tell us some real incidents where you noted a remarkable improvement in the patient’s physical state after aquatherapy?
Over the past 20 years, we have treated almost 4,000 patients.
Here’s one of the most dramatic. I have also included some of the comments we have had which we use as testimonials.
• Fourteen year-old girl was referred to our clinic in Hawaii. She was diagnosed with Aseptic bone necrosis – resulting in a non-union fracture of neck of femur (the long thigh bone).
• She was not mobile and arrived in a wheel chair.
• Because of her intolerance to even modest gravitational loads she performed all her exercises while submerged in the water, up to shoulder depth.
• As her tolerances increased she graduated to shallower depths, and eventually was able to leave the clinic six months later with only the use of a walker.
Testimonials
“I wish my doctor had sent me here first.”
-A.B. (Chronic low back pain, knee pain)
“I have spent the last ten years trying every form of therapy I could find, unsuccessfully. Prins Aquatherapy is the first that has helped. Overall, long-term, it’s working. And it’s the first thing that has.” -R.C. (Series of accidents)
“The exercise movements I participate in feel natural, and being submersed in water is relaxing. The exercise is virtually pain-free and I do not feel inhibited with the idea that I might hurt myself with any of the prescribed motions.” -A.L. (Back injury, automobile accident)
“I’m able to do more movements than I could in regular land therapy because of the support the water gives. Just being able to walk in the water without my crutches is a great relief. It has helped me strengthen and retrain my muscles in my injured leg.” -A.R. (multiple fractures of leg)
“I have been looking for a way to get back in shape without hurting myself. I had the preconception that you couldn’t exercise hard with Aquatherapy, however, with the program my Physiotherapist developed for me, when I get out of the water I know I’ve had a real workout.” -L.W. (pelvic injury)
5. How can Aquatherapy help people with autism or children with ADHD, or people with mental illness? (Since you mention in your website that you get references from psychiatrists)
We don’t know the exact causal mechanisms but it appears that the sustained, rhythmic movements have a reassuring effect on children diagnosed with Autism and ADHD. Parents report their children being a “lot calmer” for a number of hours following aquatic sessions.
In terms of Psychiatry, it is pretty well established that regular exercise is much recommended as an adjunct treatment. We can guess that the effect of exercising in the water, minimizing joint trauma and the stresses imposed by land-based exercises, are particularly suited for these patients.
Some of our most consistent referral sources were from Psychiatrists practicing in Honolulu who reported excellent feedback from their patients.
6. How long will the length of a typical aquatherapy treatment be? How do you decide the goals of aquatherapy for each patient?
Patients are usually referred for 6 initial visits. If progress is evident, as per the formal re-evaluation conducted by the treating Physical Therapist, it is not unusual for the treatment plan to include 6 or 12 more visits.
Following these additional sessions most patients are familiar with their program and are transitioned to our “maintenance” program.
7. Once the goals are achieved, is it necessary to keep getting aquatherapy to maintain the progress? Can patients do the exercises themselves once they are out of your program?
Prins Aquatherapy offers their discharged patients the opportunity to continue their exercise program at the clinic on an independent basis for a nominal fee. (called Independent Maintenance Program)
This allows the patient to have access to the equipment and the therapy pool.
8. Would the results be same from aquatherapists in any part of the world? Have your results been validated by other people?
Aquatic physical rehabilitation is now recognized and utilized as a “procedure,” rather than a modality. The increased focus can be attributed in part to its evolution from the limited confines of “Hubbard Tanks,” to the larger venues of swimming pools. These larger exercising areas accommodate a greater variety of exercises, including those that require sustained propulsive movements.
In the same way, programs that promote adult fitness have gravitated to the water to the point that there are now a large number of aquatic routines directed specifically towards the aging population.
9. About training to be an aquatherapist: what is the certification process for those who want to learn this therapy?
Licensed physical therapists in the United States have organized a sub-chapter of the APTA (American Physical Therapy Association) to increase awareness of Aquatherapy. Courses are offered to familiarize physical therapists with Aquatherapy. Some literature is available.
At our clinic we trained our clinical staff, providing the anatomical and biomechanical focus for the exercises that they would prescribe to their patients.
10. Do you undertake training for acquatherapy?
During the 22 years we have conducted our training focused on preparing our clinical staff to work with patients in the water. I have also delivered a number of lectures and presentation both nationally and internationally but these have for the most part, dealt with the overall advantages of aquatic physical therapy.
As stated in our web site, we now offer similar training, focusing on program design, specifically the anatomical and biomechanical aspects of aquatic exercises for the injured and non-injured populations.
We are in the process of putting together an interactive training DVD which will include text and accompanying video clips (primarily underwater footage). Also included with the DVD will be a manual, the primary contents will be almost 1,200 treatment protocols, divided according to treatment diagnoses, that were used at our clinic for treating patients.
11. What is the future of Aquatherapy?
With the opening of our clinic in Sri Lanka, we are getting interest from a number of Asian countries. It appears that there is now a growing awareness of the advantages of aquatic physical therapy.
12. Since Aquatherapy works partly on the principle of water reducing the gravitational effect, does it have any relevance for space medicine? For example, can Aquatherapy help prepare astronauts for extended stay in space? Can it give them an idea of the effect of weightlessness on their bodies?
Because the weightless environment in the pool necessitates different responses to motion, Astronauts, from the very outset, have been trained to move underwater. The major difference between being suspended in space vs. underwater is the presence of a viscous medium with provides resistance which is non-existent in space. Treatments in the two environments may have as many differences as similarities. Perhaps this would be a fruitful area of investigation once we establish permanent space stations and can shuttle the general population back and forth.
The major task for the space program has been to design exercise protocols for astronauts that will provide adequate strength and cardiovascular responses during prolonged stints in a weightless environment. As far as I know, this research is on-going.
13. How did you get so involved in this field of Aquatherapy?
In 1986, as the director of the Aquatic Research Laboratory at the University of Hawaii, I was awarded a federal grant through the National Institute for Disability Rehabilitation & Research, U.S. Department of Education.
The study investigated the underwater movement mechanics of persons with permanent physical disabilities. This was the first time a detailed analysis was conducted and generated interest from the medical profession here in Honolulu, and elsewhere.
The result was that a number of orthopedic surgeons and neurologists in Honolulu encouraged me to start an Aquatherapy business. Since I am not a physical therapist, my training and expertise is in biomechanics as it deals with human motion in the water, my goal was to design a battery of exercises that can be used by clinicians for treating patients. Being afforded the opportunity to work with patients, who for the most part reported making good progress, particularly since they had tried traditional land-based physical therapy without success, allowed me to fine tune the protocols, and within a year, hire a clinical staff to open a formal aquatic physical therapy clinic.
The Honolulu clinic was in business from 1989 to 2008. Our referral base was approximately 230 medical practitioners, specializing in a wide range of specialties. We closed the clinic in the spring of 2008. We shipped the equipment to Colombo, and now have registered physiotherapists treating patients following the program we developed.
We believe our system, particularly the training and familiarization with the different aquatic exercises and protocols for the varied diagnoses can be employed at any location where a suitable pool can be either constructed or modified for clinical use.
14. In the end can I request you to give a brief synopsis of biomechanical reasons that make Aquatherapy so effective.
• The aquatic environment reduces the effect of gravity, allowing patients to begin an exercise program without increasing pain levels or stress on painful joints.
• The support of the water allows patients to increase their range of motion while strengthening weakened muscles
• Rhythmic movements, such as walking at various depths, aqua jogging, and swimming, enable patients to safely improve their cardiovascular endurance and increase fitness.
• The variable resistance of the water accommodates a full range of exercise intensities from gentle exercise for the newly injured to vigorous exercise for the more athletic individual.
• Water exercises are beneficial for recovery from acute and chronic injury as well as pre- and post-surgery (examples such as hip or knee replacements).
Source-Medindia
Dr. Susan/L