Coordinated Care and therapeutic lifestyle changes improve the condition of patients with diabetes and depression.

‘Collaborative care model approach shows improvements in more than 70% of the people with diabetes and depression. The study shows the strength of integrated approach with a little bit of therapeutic lifestyle changes.’
Read More..




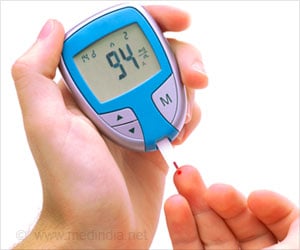
Researchers from Emory University, University of Washington School of Medicine, and their colleagues in India compared a collaborative care model with usual care in 404 patients with diabetes and moderate-to-severe depressive symptoms. Read More..
More than 70 percent in the group receiving the integrated approach had improvements in diabetes and depression.
The results of the In the INDEPENDENT (Integrating Depression and Diabetes Treatment) study show the strength of coordinated care and a little therapeutic lifestyle changes (TLC).
“Too often, mental health is overlooked due to fragmented care, stigma of psychiatric illnesses, and shortages of mental health professions,” said first author Mohammed Ali, vice chair of family and preventive medicine at Emory University.
Ali said that depression worsens patients’ likelihood of managing their diabetes well. Poorly controlled diabetes can result in higher risk of heart attacks and other diabetes complications and greater mortality.
Advertisement
The model in the study was adapted from a collaborative-care model developed by the late Wayne Katon, vice chair of psychiatry and behavioral sciences at the University of Washington School of Medicine. Katon developed an influential research program on the effects of depression on physical health.
Advertisement
“The real power of this model is bringing mental health care to people who cannot access it elsewhere,” said Chwastiak. “What is most exciting is that this model might be an effective strategy for addressing severe health workforce shortages.”
Chwastiak led training of 10 nutritionists who worked in four diabetes clinics to be patient-care managers. The care managers worked with patients, their family members and doctor and a consulting psychiatrist on an individualized treatment plans. The patient care manager advocated for the patient and supported them to manage their illness more effectively.
“The relationship with the patient care manager was so powerful,” said Chwastiak. “The patients were very attached to them.”
Senior author Viswanathan Mohan, chairman of Dr. Mohan’s Diabetes Specialties Centre and director of Madras Diabetes Research Foundation in India, called the findings impressive.
“This was the first study reporting on whether a one-year integrated, collaborative care model has sustainable effects at two years,” said Mohan. “This low-cost model produced impressive results both in improving depression as well as in several metabolic parameters and can be useful in other settings and countries.”
Contributing authors also included K.M. Venkat Narayan, and Shivani Patel from Emory University. The study was funded by the National Institute of Mental Health.
Source-Newswise