‘World Health Organization recommends that countries start patients immediately on ART regardless of CD4 count.’
Tweet it Now
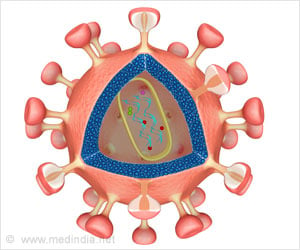
"Treatment outcomes are a result of both biological efficacy and patient behavior. Extending HIV treatment eligibility to patients at diagnosis substantially increases retention in care, an effect not observed in prior trials." says lead author Jacob Bor, assistant professor of global health at BUSPH. In the past, ART eligibility was determined based on the CD4 cell count in patients diagnosed with HIV. Now, however, the World Health Organization recommends that countries start patients immediately on ART regardless of CD4 count. Understanding the expected benefits of this "treat all" approach, the authors wrote, is particularly important for countries like South Africa, where HIV remains the leading cause of death and disability despite the mass provision of treatment.
"Patients denied therapy under older guidelines often dropped out of care altogether, leading to worse outcomes," says Bor. "We show that extending HIV treatment eligibility to these patients significantly increased their chances of staying in care."
The researchers assessed the association between immediate versus deferred therapy and the subsequent rate of patients lost from HIV care among 11,306 patients in a large public-sector treatment program in rural South Africa. Using a regression-discontinuity design, they compared 12-month retention in care among patients presenting just below the threshold for ART eligibility (350-cells/μl CD4) versus those presenting just above.
The researchers found that patients who were immediately eligible for ART at diagnosis were 25 percentage points more likely to start therapy and 18 percentage points more likely to remain in clinical HIV care at 12 months compared to patients who were not eligible for immediate therapy. Among patients whose treatment decision was based on their CD4 count, having an eligible CD4 count increased their 12-month retention rate from 21 percent to 91 percent, a 70 percentage-point increase.
Advertisement
Advertisement