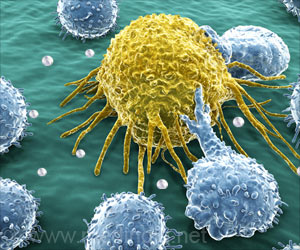
‘Since tumur cannot grow beyond a certain size or spread without a blood supply, scientists are trying to find ways to block tumor angiogenesis.’
Tweet it Now
"Deciphering and targeting mechanisms involved in resistance to anti-angiogenic therapy is critical to realizing the full potential of this promising cancer therapy," says Dai Fukumura, MD, PhD, deputy director of the Steele Labs, co-senior author of the paper. "Not only is this the first report investigating the role in anti-angiogenic cancer therapy of a subset of innate immune cells - Ly6Clow or non-classical monocytes - it is also the first to find an immunosuppressive function for these cells and to identify that as the key mechanism conferring resistance to anti-angiogenic therapy." Angiogenesis inhibitors - often given in combination with traditional therapies - can improve treatment for several types of cancer, both by restricting the growth of new blood vessels and by "normalizing" the abnormal vessels in and around a tumor that can interfere with both chemotherapy and radiation therapy. But resistance to anti-angiogenic therapy limits the drugs' survival benefits. Several studies have suggested a role in the development of resistance for the immune system - particularly innate immune cells that suppress immune activity. But how specific subsets of these cells contribute to resistance has not been defined.
A series of experiments in mouse models of colorectal cancer first revealed that treatments blocking the vascular endothelial growth factor (VEGF) pathway - the target of approved anti-angiogenic drugs - induce the accumulation of monocytes and neutrophils. It soon became apparent that the buildup of non-classical monocytes - a subset previously identified as patrolling healthy blood vessels and possibly having an anti-tumor effect in lung cancer - was responsible for development of an immunosuppressive tumor microenvironment in colorectal cancer.
The research team identified the signaling pathway by which VEGF blockade induces expression of a molecule called CX3CL1 on tumor cells, attracting non-classical monocytes that carry the matching receptor. Those cells, in turn, attract neutrophils with another molecule called CXCL5; and both immune cells express factors that inhibit the proliferation of T cells, reducing the overall immune response to the tumor. Examination of biopsy samples taken from human patients before and after anti-angiogenic therapy revealed that expression of these chemokines - molecules that attract immune cells - increased in response to anti-VEGF treatment.
Since several methods of experimentally blocking the pathway improved the effects of anti-VEGF therapy in the mouse models, the team collaborated with Massachusetts Institute of Technology investigators to develop a potential gene therapy approach. Utilizing nanoparticle-delivered RNA interference against the interaction between CX3CL1 and its receptor, the approach significantly reduced the infiltration of non-classical monocytes into treated tumors and increased the beneficial effects of anti-VEGF therapy in a mouse model.
Advertisement
Rakesh K. Jain, PhD, director of the Steele Labs and co-senior author of the Journal of Clinical Investigation report, adds, "Tumors also escape the immune system through immune checkpoint molecules like PD-1 and CTLA-4, which are the targets of recently approved drugs. But that strategy has been effective only in some tumor types and in only a fraction of patients. Therapeutic strategies based on our findings regarding the immunosuppressive action of non-classical monocytes may prove to have synergistic effect with those approved immune checkpoint inhibitors." Jain is the Cook Professor of Radiation Oncology (Tumor Biology) at HMS.
Advertisement












