"The significant drug discovery advances presented today represent our continued progress in fighting resistant disease, identifying and disabling cancer gene signaling, and improving outcomes in patients who struggle with poor prognoses and few treatment options," said Aaron Schimmer, MD, PhD, moderator of the press conference and Clinician Scientist at the Princess Margaret Cancer Centre, University Health Network in Toronto. "Considering the incredible progress we have made over just a few years, I am encouraged and excited to see what the next decade has in store, and how the next generation of therapies will further help us conquer blood cancers and save lives."
Final Results of a Phase II Open-Label, Monotherapy Efficacy and Safety Study of Quizartinib (AC220) in Patients with FLT3-ITD Positive or Negative Relapsed/Refractory Acute Myeloid Leukemia After Second-Line Chemotherapy or Hematopoietic Stem Cell Transplantation
Research suggests that a new targeted therapy, quizartinib, may be a safe and effective option to treat a subset of patients with treatment-resistant acute myeloid leukemia (AML).
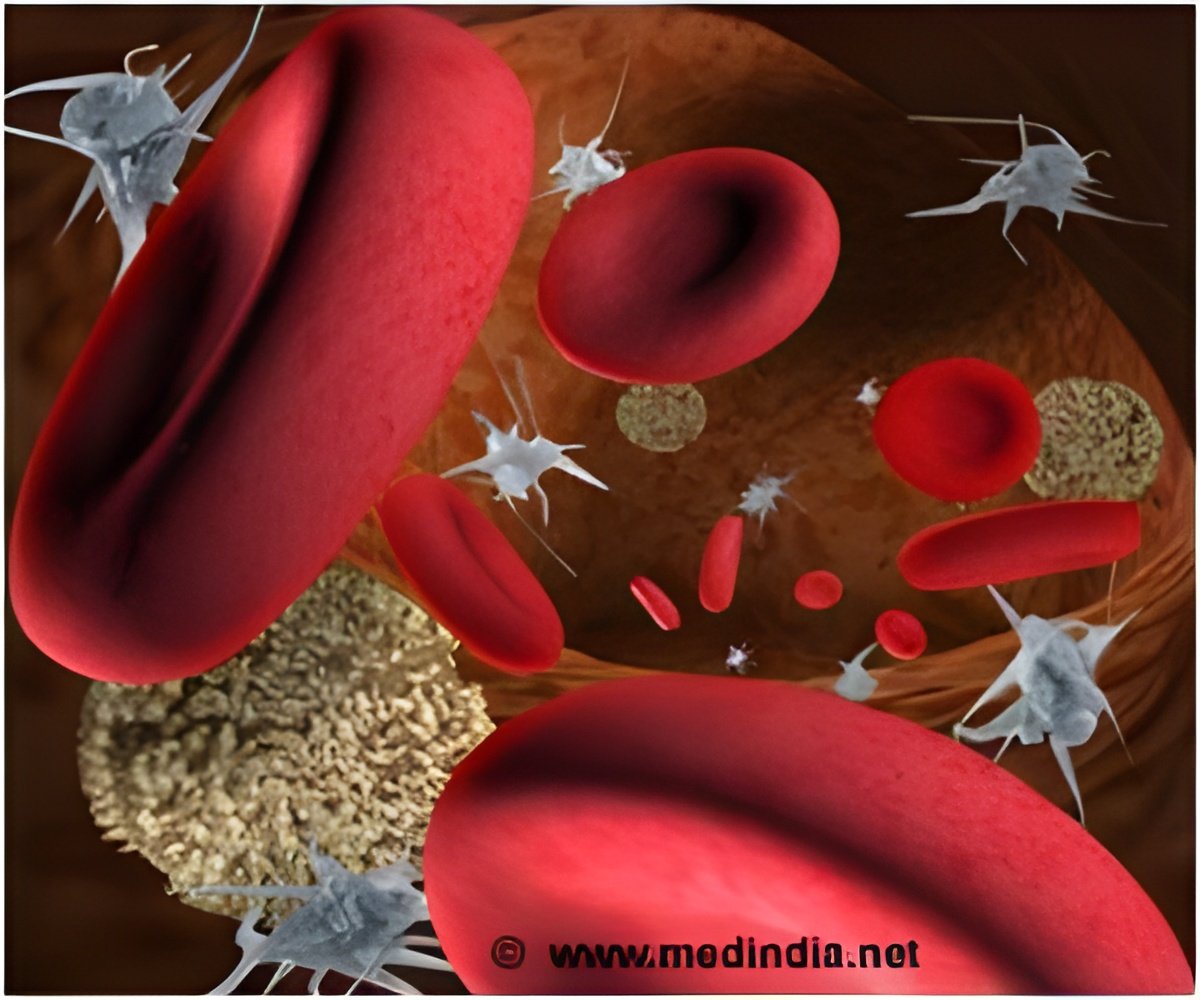
AML is a fast-growing blood cancer in which patients produce an excessive amount of abnormal, immature white blood cells that are unable to adequately fight infection. Following AML diagnosis, leukemia cells from patients undergo genetic testing to identify the mutation driving the disease, which helps determine the appropriate treatment protocol. Of the many types of genetic mutations that can occur in AML, one of the most threatening is the FLT3-ITD (internal tandem duplication), which makes the leukemia even more aggressive and typically leads to failure of standard chemotherapy treatment response.
"The FLT3 mutation is essentially a power switch that leukemia cells use to spread more aggressively, which helps them to grow back immediately after chemotherapy," said Mark J. Levis, MD, PhD, lead author and Associate Professor of Oncology, Pharmacology, and Medicine at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins Medicine in Baltimore. "The only way to treat this type of mutation is to find a way to turn the switch off — a feat that has eluded researchers for far too long."
Advertisement
In order to assess the efficacy and safety of quizartinib as a single agent (drug used alone in treatment) in AML patients with the FLT3-ITD mutation, researchers conducted a Phase II study among 333 patients that were divided into two treatment cohorts. Cohort 1 consisted of patients age 60 or over with the FLT3-ITD mutation who failed to achieve remission with standard chemotherapy, or who had recently relapsed for the first time. Cohort 2 consisted of patients over age 18 with the FLT3-ITD mutation who presented with relapsed or refractory AML and had been administered salvage chemotherapy after failing to respond to prior treatment, or had relapsed after a stem cell transplant. Most patients in this study had the FLT3-ITD mutation, but a small number in each cohort lacked the mutation.
Advertisement
Following one to three cycles of quizartinib treatment, researchers observed a CRc rate of 44 percent (4% CR, 0 CRp, and 40% CRi) in patients with the FLT3-ITD mutation with a median duration of response of 11.3 weeks and median overall survival of 23.1 weeks. In patients without the mutation, researchers observed a 34 percent CRc rate (3% CR, 3% CRp, and 29% CRi) with a median duration of response of five weeks and median overall survival of 25.6 weeks. Of those patients in both cohorts who did not respond to their last AML therapy, 47 percent of those with FLT3-ITD and 31 percent of those without achieved a CRc with quizartinib. In both cohorts, 34 percent of patients were successfully bridged to a potentially curative allogeneic transplant.
Common adverse effects of treatment with quizartinib (observed in more than 20% of patients) included QT prolongation (26%), a heart complication associated with some medications and managed by reducing dosage, as well as nausea (38%), vomiting (26%), anemia (29%), fever (25%), diarrhea (20%), and fatigue (20%). These results demonstrate that quizartinib can produce a high treatment response rate in a group of very poor-prognosis AML patients with the FLT3-ITD mutation with manageable toxicity.
"Quizartinib is the first and only single-agent drug that has produced a clinical benefit in AML patients with this deadly mutation who have failed previous therapy," said Dr. Levis. "The number of patients bridged to a stem cell transplant was very significant. We plan on using these encouraging results to design and conduct additional randomized trials that will hopefully lead to the approval of quizartinib to make it accessible to those patients who previously had no hope for a cure."
Researchers have demonstrated that combination therapy with PU-H71 and ruxolitinib increases the durability and effectiveness of a treatment that had previously shown limited utility for patients with myelofibrosis.
Myelofibrosis is a chronic malignant blood disorder commonly caused by mutations in the JAK2 pathway (which normally signals the body to create blood cells), including most commonly the JAK2 V617F mutation. This mutation leads to the overproduction of scar tissue in the bone marrow and shifts red and white blood cells and platelets from the bone marrow into the spleen and liver, enlarging the organs and leading to anemia, infection, inflammation, and easy bleeding and bruising.
The first approved treatment for myelofibrosis is ruxolitinib, a therapy that targets the JAK2 mutation by blocking the action of all JAK-related genes in the body, including those from both healthy and diseased cells. However, clinical results have been modest to date. In particular, resistance to JAK inhibitors has been associated with an increase in JAK2 levels, which leads to continued JAK2 activity despite ruxolitinib treatment. This resistance can be reversed by inhibiting heat shock protein 90 (HSP 90), which destabilizes JAK2 and reduces JAK2 protein levels. Since cancer cells are continually dividing, they constantly burden the cell system and depend on HSP90 function to allow the JAK2 protein to maintain cancer cells' function and growth.
Recognizing HSPs as a potential target for treatment, researchers have recently explored the possibility of blocking HSP90 to treat blood cancers. Unlike ruxolitinib, which blocks the function of the abnormal JAK2 protein that maintains the function of the cancerous cell, HSP90 inhibitors block the function of HSP90 in the cells. This allows for the breakdown of the JAK2 protein and weakens the cell's ability to grow and divide, allowing it to become sensitive to treatment. PU-H71, a HSP90 inhibitor, previously shown to have efficacy in different cancer cells and animal models including myelofibrosis, is currently undergoing Phase I clinical trials.
One emerging hypothesis is that combining the JAK2 inhibitor ruxolitinib with HSP90 inhibitors may increase the efficacy of myelofibrosis treatment. To test this hypothesis, a team of investigators treated mice that had myelofibrosis with the investigational combination therapy, comparing their results to control groups treated with ruxolitinib alone or PU-H71 alone. They also assessed the effects of adding PU-H71 treatment as a second therapy to mice already being treated with ruxolitinib. Study endpoints included reduction in white blood cell count, platelet count, and spleen weight; reduction in JAK2 protein levels in the blood, spleen, and bone marrow; and presence of scar tissue in the bone marrow.
In this study, researchers observed that mice that had been treated with the combination therapy had a more significant reduction in white blood cell count, platelet count, and spleen weight after 14 days of therapy. The benefits of combination therapy versus ruxolitinib alone were even more significant after 29 days of treatment. The combination therapy was also associated with a reduction in bone marrow scar tissue and a reduction in the activity of the JAK2 pathway. Comparable effects were also observed in mice that were treated with PU-H71 plus ruxolitinib after initial monotherapy with ruxolitinib, further demonstrating the efficacy of combination treatment. Most importantly, in those mice treated with combination ruxolitinib and PU-H71 therapy, investigators observed a decrease in JAK2 levels, revealing that PU-H71 may prevent or reverse the increases in JAK2 protein levels seen with chronic ruxolitinib therapy. Of note, combination treatment was well tolerated and not associated with increased side effects compared to either therapy alone.
"Now that we have found a way to combat the treatment resistance commonly seen in myelofibrosis, we are continuing these trials with the hope that these results will one day provide a treatment option superior to what is currently available for these patients," said Priya Koppikar, PhD, second author and research scholar in the Human Oncology and Pathogenesis Program (HOPP) at Memorial Sloan-Kettering Cancer Center in New York.
"We believe these results provide the impetus for the first studies combining ruxolitinib with HSP90 inhibitors in myelofibrosis patients, and we are working to begin these trials as soon as possible to improve their outcomes," added Ross Levine, MD, lead author and Associate Attending Physician in the HOPP and Leukemia Service at Memorial Sloan-Kettering Cancer Center in New York.
A Pivotal Phase II Trial of Ponatinib in Patients with Chronic Myeloid Leukemia (CML) and Philadelphia Chromosome-Positive Acute Lymphoblastic Leukemia (Ph+ALL) Resistant or Intolerant to Dasatinib or Nilotinib, or with the T315I BCR-ABL Mutation: 12-Month Follow-up of the PACE Trial
Researchers have discovered that ponatinib, a new oral tyrosine-kinase inhibitor (TKI), can silence a deadly mutation in chronic myeloid leukemia (CML) and Philadelphia chromosome-positive acute lymphocytic leukemia (Ph+ALL).
CML and Ph+ALL are leukemias caused by an abnormality known as the Philadelphia chromosome that produces the cancer-causing gene BCR-ABL. This gene provides the DNA code to produce the BCR-ABL tyrosine-kinase, a protein found on the leukemia cell surface critical to its development.
Source-Eurekalert