Highlights
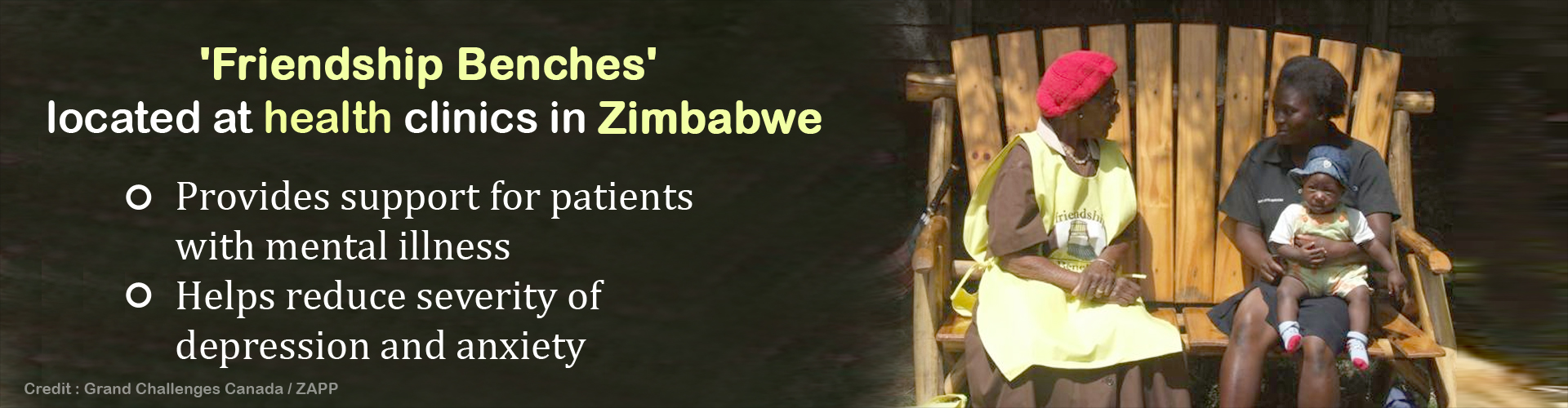
- An innovative approach called ‘Friendship Bench’ located at health clinics in developing countries was found to improve mental health of millions of people.
- Friendship Benches are wooden seat offices aimed to support patients living with anxiety, depression and other common mental disorders.
- Over 27,500 people have accessed Friendship Bench therapy in sub-Saharan Africa.
A randomized controlled trial was conducted by the University of Zimbabwe, the London School of Hygiene & Tropical Medicine and King's College London, to find the effect of the innovative approach. The study was funded by the Government of Canada through Grand Challenges Canada.
The study found that problem-solving therapy through Friendship Benches can significantly improve the lives of millions of people with moderate and severe mental health problems.
Patients who had six weekly problem-solving therapy sessions on the Friendship Benches showed significant differences in severity of depression, anxiety and suicidal thoughts.
The research team used locally validated questionnaires for depression and anxiety: the Shona Symptom Questionnaire (SSQ), the Patient Health Questionnaire (PHQ) and the Generalized Anxiety Disorder scale (GAD).
The patients were four times less likely to have anxiety symptoms and five times less likely to have suicidal thoughts when compared with the patients in the control group.
Based on the PHQ, about 50 percent of the patients who received standard care still had symptoms of depression compared to 14 percent of patients who received through Friendship Benches.
Based on GAD, nearly 48 percent of patients who received standard care still had symptoms of anxiety compared to 12 percent who received treatment through Friendship Benches.
Based on SSQ, about 12 percent of the patients who received standard care still had suicidal thoughts compared to 2 percent who received treatment through Friendship Benches.
The Friendship Bench intervention was also shown to be well suited to improve health outcomes among highly vulnerable individuals. About 86 percent of the study's participants were women, over 40 percent were HIV positive, and 70 percent had experienced domestic violence or physical illness.
Lead author of the study Dr. Dixon Chibanda, a consultant psychiatrist in Harare, co-founded the Friendship Bench network in response to the appalling shortage of evidence-based treatment for people with mental disorders in Zimbabwe, a problem common throughout Africa.
While about 25 percent of the country's primary care patients suffer from depression, anxiety and other common mental disorders, Zimbabwe (population 15 million) has only 10 psychiatrists and 15 clinical psychologists.
"Common mental disorders impose a huge burden on all countries of sub-Saharan Africa," says Dr. Chibanda. "Developed over 20 years of community research, the Friendship Bench empowers people to achieve a greater sense of coping and control over their lives by teaching them a structured way to identify problems and find workable solutions."
With CDN $1 million in funding from Grand Challenges Canada earlier this year, the Friendship Bench has since been scaled to 72 clinics in the cities of Harare, Gweru and Chitungwiza (total population 1.8 million). Through collaborating with a Médecins Sans Frontières psychiatric program in Zimbabwe, the Friendship Bench is working to create the largest comprehensive mental health program in sub-Saharan Africa.
To date, over 27,500 people have accessed treatment.
"In developing countries, nearly 90 percent of people with mental disorders are unable to access any treatment," says Dr. Peter A. Singer, Chief Executive Officer of Grand Challenges Canada. "We need innovations like the Friendship Bench to flip the gap and go from 10 percent of people receiving treatment, to 90 percent of people receiving treatment."
"In many parts of Africa, if you are poor and mentally ill, your chances of getting adequate treatment are close to zero," says Dr. Karlee Silver, Vice President Programs at Grand Challenges Canada. "In Zimbabwe, that's changing thanks to the Friendship Bench, the first project with the potential to make mental health care accessible to an entire African nation."
In 2017, the team will focus on expanding the model to reach other vulnerable populations, including youth and refugees. In partnership with the Swedish NGO SolidarMed, the team intends to expand implementation of this model in Masvingo province and subsequently in the refugee centres of the eastern highlands on the border with Mozambique.
"The Friendship Bench team, working with the Zimbabwe Ministry of Health, has been able to substantially scale up services for some of the most deprived people in the community," says Dr. Shekhar Saxena, Director of Mental Health and Substance Abuse at the World Health Organization. "By supporting the uptake of mental health innovations like the Friendship Bench, Canada is helping to turn the tide in the global mental health challenge."
Reference:
- Dixon Chibanda, Helen A. Weiss, Ruth Verhey, MSc1; et al Victoria Simms, Ronald Munjoma, Simbarashe Rusakaniko, Alfred Chingono, Epiphania Munetsi, Tarisai Bere, Ethel Manda, Melanie Abas, Ricardo Araya. ‘Effect of a Primary Care–Based Psychological Intervention on Symptoms of Common Mental Disorders in Zimbabwe: A Randomized Clinical Trial,’ Journal of the American Medical Association (JAMA). (2016);316(24):2618-2626.DOI:10.1001/jama.2016.19102
Source-Medindia