- The 2018 updated guideline for the clinical management of blood cholesterol has been published
- The guideline provides recommendations on how to manage blood cholesterol in high-risk patients suffering from atherosclerotic cardiovascular disease (ASCVD)
- Management of blood cholesterol in ASCVD patients could prevent many deaths arising from heart disease
This guideline has been co-published in the American College of Cardiology’s Journal of the American College of Cardiology (JACC) and the American Heart Association’s journal, Circulation.
Read More..
What’s New in the 2018 Guideline?
The ACC/AHA cholesterol management guideline framed in 2013 advised that the focus should be on high-intensity statin therapy and not on reduction of low-density lipoprotein (LDL) levels. However, the 2018 updated guideline reverts to the initial LDL-lowering goals. It emphasizes that lipid management is the key to reducing the risk of atherosclerotic cardiovascular disease (ASCVD). It also lays stress on a more intensive therapeutic approach, based on the latest evidence generated by recent randomized controlled clinical trials on new lipid-lowering drug molecules. Moreover, it also provides guidance on coronary artery calcium (CAC) testing and personalized risk assessment. This guideline will be of particular benefit for those patients who need primary or secondary prevention for ASCVD.What is Atherosclerotic Cardiovascular Disease (ASCVD)?
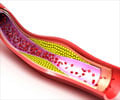
ASCVD occurs by a process called atherosclerosis. It is a condition in which the arteries become hardened and stiff due to the deposition of cholesterol and cellular debris along the inner walls. These deposits of cholesterol, macrophages, calcium and other substances from the blood are collectively called plaque.As a result, with plaque build-up, the lumen of the arteries become narrowed and hinders the smooth flow of blood. Sometimes, the plaque can grow to such an extent that it clogs up the arteries. This can cause the formation of blood clots that can lead to very serious, life-threatening conditions such as stroke and heart attack.
What are the Major Recommendations?
The key recommendations have been summarized below:- More emphasis should be laid on a healthy lifestyle throughout life as this is essential for the primary prevention of ASCVD by significantly reducing the risk factors.
- In the case of patients with clinical ASCVD, low-density lipoprotein (LDL) should be reduced by the administration of high-intensity statins or its maximum tolerated dose. Maximally tolerated statin dose should aim to reduce LDL levels by ≥ 50 percent.
- In the case of very high-risk ASCVD, the LDL threshold should be at 70 mg/dL (milligrams per deciliter) in order to consider adding non-statin therapies to existing statins. If LDL remains ≥ 70 mg/dL in very high-risk ASCVD patients, it will be prudent to add ezetimibe to the maximally tolerated statin dose. However, if the LDL levels remain ≥ 70 mg/dL in these very high-risk patients, in spite of maximally tolerated statin plus ezetimibe, adding a PCSK9 inhibitor would be advisable.
- In case of patients suffering from severe primary hypercholesterolemia (LDL ≥ 190 mg/dL), high-intensity statin therapy should be started without calculating the 10-years ASCVD risk. If LDL levels remain ≥ 100 mg/dL, ezetimibe should be added. Moreover, if the LDL levels remain ≥ 100 mg/dL, in spite of statin plus ezetimibe and the patients have multiple risk-factors for developing ASCVD, then adding a PCSK9 inhibitor would be advisable.
- In case of diabetic patients in the age group 40-75 years, who have LDL ≥ 70 mg/dL, moderate-intensity statins should be started without calculating the 10-year ASCVD risk. Diabetic patients at higher risk, especially with multiple risk-factors, should preferably receive high-intensity statins to lower the LDL levels by 50 percent or more.
- A doctor-patient discussion on risk assessment prior to starting statins is recommended for patients in the age group 40-75 years, who have been evaluated for primary ASCVD prevention. The following discussion points should be kept in mind:
- Review of major risk factors – (i) smoking, (ii) hypertension (high blood pressure), (iii) LDL, (iv) HbA1c (glycosylated hemoglobin), (v) calculated 10-year ASCVD risk
- Presence of risk-enhancing factors (see # 8)
- Potential benefits of lifestyle and statin therapy
- Potential for adverse effects and drug interactions
- Cost of statin therapy
- Patient’s contribution/role in shared decision-making
- In case of non-diabetic patients in the age-group 40-75 years having LDL ≥ 70 mg/dL and 10-year ASCVD risk ≥ 7.5 percent, moderate-intensity statins should be started if statin therapy emerges as an option, following doctor-patient discussion.
- In case of non-diabetic patients in the age-group 40-75 years having 10-year ASCVD risk between 5-19.9 percent, statin therapy should be started if risk-enhancing factors are present. The following risk-enhancing factors should be taken into consideration:
- Family history of premature ASCVD
- Persistently elevated LDL levels ≥ 160 mg/dL
- Persistently elevated triglycerides (TGL) levels ≥ 175 mg/dL
- Metabolic syndrome
- History of preeclampsia at age < 40 years
- History of premature menopause at age < 40 years
- Chronic kidney disease (CKD)
- Chronic inflammatory disorders – (i) rheumatoid arthritis, (ii) chronic HIV infection, (iii) psoriasis
- High-risk ethnic groups e.g. South Asians
- In case of non-diabetic patients in the age-group 40-75 years having LDL levels between 70-89 mg/dL and 10-year ASCVD risk between 7.5-19.9 percent, if a decision on statin therapy can’t be taken, the coronary artery calcium (CAC) should be measured. Based on the following CAC scores (measured in Agatston units), a decision on statin therapy can be made:
- CAC score 0 – Statin to be withheld or delayed. Exceptions include (i) smokers, (ii) diabetics, (iii) those with a strong family history of premature ASCVD
- CAC score 1-99 – Statin therapy favored, especially in patients > 55 years of age
- CAC score ≥ 100 or ≥ 75th percentile – Statin therapy indicated, unless postponed by the outcome of the doctor-patient discussion on ASCVD risk
- An assessment should be made with reference to (i) adherence to therapy and (ii) percentage response to therapy, with reference to lipid-lowering drugs and lifestyle modifications. Lipid profile should be measured every 1-3 months after starting statin therapy or after dose adjustment and should be repeated every 3-12 months as required.
Funding Source
The framing of the guideline was funded by the American College of Cardiology (ACC), the American Heart Association (AHA), and 10 other clinical organizations.Reference:
- 2018 Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines - (http://www.onlinejacc.org/content/accj/early/2018/11/02/j.jacc.2018.11.003.full.pdf)
Source-Medindia