Highlights
- Mini stomach tissue grown in the lab, provides better understanding of developing stomach from stem cells.
- The mini stomach was found to produce acid as well as digestive enzymes.
- Mini stomach and the previously grown mini intestine can be used to understand gastrointestinal mobility as well as digestive processes.
Dr. Jim Wells who is the principal investigator for the study stated that now that they could grow both the antral and the corpus/ fundic type gastric mini organs of humans,It is therefore possible to study interactions between human gastric tissues and identify how they will react to infection, damage as well as to drugs. Such information can be used to study diseases that affect the stomach and also identify the pathway involved in gastric cancer..
The latest study is a continuation of studies that began in the year 2010 by a research team led by Dr. Well when pluripotent stem cells were used to grow human stomach and intestines. The tissues are being used to identify the causes as well as possible treatment involved in human gastrointestinal tract.
As a part of their previous study, the scientists grew human intestine that included an enteric nervous system. These tissues are highly functional and were able to absorb nutrients and display peristalsis, which is the distinctive movement of the intestine to move the food from one end of the GI tract to the other.
Dr. Well’s laboratory is also looking intently at understanding how embryonic development which includes the development of stomach, pancreas, esophagus and intestines. The data obtained can also be used for devising treatment strategies for genetic diseases that include Hirschsprung’s disease as well as monogenic diabetes.
Beginning of the Study
The growth of mini organs in the lab, also called organoids or miniature versions of organs was initially a daunting task as it posed a lot of conditions. The first step was to identify a culture medium into which mechanical constraints could be applied for the development of the different cells in the organ from stem cells so that they can be organized into layers to form an organ-like structure as opposed to a simple layer of cell aggregates.The research team under Dr. Well lacked a basic understanding of how stomach developed from the embryonic stage which was a significant challenge for the team. Dr. Wells explained that they could not grow stomach tissue in the Petri dish without first identifying how the stomach grows from the embryo.
WNT/β-catenin
The scientists, using their study on mice, found out that there was a basic genetic pathway WNT/β-catenin which was vital in determining the development of the corpus/fundus region of mouse stomach tissue that were developed from mouse embryos. This study was used to alter the WNT/β-catenin pathway to grow human fundus mini organs which were developed form pluripotent stem cells.Refining the Process
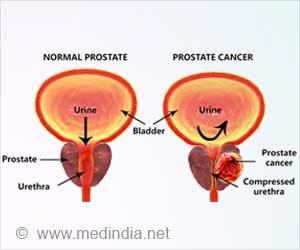
Dr. Wells and his research team then refined the growth and development process by identifying other pathways which could induce the formation of vital stomach cell types of the fundus region. The cell types that were developed also included major cells like the cells that were involved in the production of the key digestive enzyme pepsin along with parietal cells. The parietal cells are involved in the secretion of hydrochloric acid that is essential for digestion and is also an intrinsic factor that aids the intestines in the absorption of vitamin B-12. This is a key step that is necessary for the production of blood cells as well as for the development of a nervous system which is healthy.When asked how long it took for the stem to grow into gastric-fundus tissues in a Petri-dish, Dr. Wells responded by saying that it took six weeks.
Benefits of the Study
- Provides a chance to study the development of the stomach tissue from stem cells
- It can be used to study gastric cancer in humans
- It can be used to understand how the organoids will respond after infection with Helicobacter pylori (H.pylori)
- H. pylori can lead to the development of stomach ulcers, chronic gastritis and increase the risk for stomach cancer
References:
- Scientists create “mini-organs” in vitro - (http://www.genethique.org/en/scientists-create-mini-organs-vitro-63700.html#.WGyQcFN97IU)