Highlights
- Retinal degeneration is a hereditary condition, characterized by death of photoreceptor cells, eventually leading to blindness.
- New research states some success in transplanting 3D retinal sheets derived from embryonic pluripotent stem cells to restore vision.
- Normal vision can be restored by forming structured outer nuclear layers in the retina which are lost in end-stage retinal degeneration.
Futile Graft Photoreceptor Transplant
In end-stage retinal degeneration, the outer nuclear layer of the retina is completely missing and most of the photoreceptors are dead. As a result, the neurons do not have any input and no signals are carried to the brain.There have been many attempts to treat the disease through retinal transplants.
Some studies have also shown that transplanting graft photoreceptors to the host cells can rescue retinal function. Host cells are the bipolar retinal cells. They exist between the photoreceptor cells and ganglion cells.They send signals to the brain via ganglion cells.
But, to date, there has been no success in transplanting photoreceptors that functionally connect to host cells and send visual signals to host retinal and brain.
3D Retinal Sheets
The research team led by Masayo Takahashi and Michiko Mandai of the RIKEN Center for Developmental Biology studied end-stage retinal degeneration using a mouse model.The team has shown that to restore normal structure connectivity in the retina, 3D retinal sheets derived from mouse induced pluripotent stem cells (iPSCs) can be used.
When transplanted into mice with end-stage retinal degeneration, the iPSC-derived retinal tissue developed to form photoreceptors that established direct contact with neighboring host cells in the retina.
"Using this method was a key point," explains first author Michiko Mandai, "Transplanting retinal tissue instead of simply using photoreceptor cells allowed the development of more mature, organized morphology, which likely led to better responses to light."
After integrating some modifications to both the retinal sheets and the model mice, the research team assessed the success of transplantation.
The ends of the photoreceptors connect to the host neurons, which are the bipolar retinal cells and they send visual signals to the brain.
The research team used a fluorescent protein to label the ends of the photoreceptors. Another fluorescent protein was used to label the host retinal bipolar cells.
They found that the labeled cell terminals from the graft did indeed make contact with the cells labeled in the host, indicating that the newly grown photoreceptors naturally connected themselves to the bipolar cells in the model mice.
Testing Vision
Mice with normal vision can learn to associate sounds or light with different events, the same way that Pavlov's famous dog associated food with the sound of a bell.To assess whether the mice could see light, the researchers used this behavioral learning task.
Before surgery, the model mice that lacked a photoreceptor layer in their retinas could not learn to associate anything with light. But after the transplant, they were able to learn, provided that a substantial amount of the transplant was located in the correct place.
This means that not only did the new cells in the retina respond to light, but the information traveled to the brain and could normally be used to learn.
"These results are a proof of concept for using iPSC-derived retinal tissue to treat retinal degeneration," says Mandai.
The research team cautioned that this therapy is still at its developmental stage. "We cannot expect to restore practical vision at the moment," Mandai explains. "We will start from seeing a simple light, then possibly move on to larger figures in the next stage."
To make the findings more human-friendly before clinical trials, the team hopes to conduct a few more studies using human iPSC-derived retinal tissue in animals with end-stage retinal degeneration.
Clinical trials are the only way to determine how many new connections are needed to restore vision.
Photoreceptor Cells in the Eye
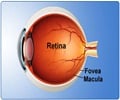
A photoreceptor cell is a specialized type of neuron found in the retina. Photoreceptors absorb and convert light into electrical signals.These signals are sent to other cells in the retina and ultimately through the optic nerve to the brain where they are processed into the images.
The two classic photoreceptor cells are rods and cones.
- Rods are rod-shaped cells in the outer regions of the retina that are responsible for peripheral and night vision.
- Cones reside mostly in the central portion of the retina, and are responsible for central vision and color perception.
Retinal Degeneration
There are two types of degenerative conditions of the retinaAge-Related Macular Degeneration (AMD)
AMD is a degenerative eye condition, leading to loss of vision among people aged 50 and older. It causes damage to the macula, a small spot near the center of the retina.AMD may advance slowly or rapidly and the loss of vision depends on the disease progression.
The common symptom of AMD is blurred area near the center of vision, which progresses to a blank spot. Over time, the blurred area may grow larger and objects also may not appear to be as bright as they used to be.
The loss of central vision in AMD interferes with simple everyday activities, such as the ability to see faces, drive, read, and write.
Retinitis Pigmentosa
Retinitis pigmentosa (RP) refers to a group of inherited diseases caused by gene mutations. It is inherited from one or both parents.An estimated 100,000 people in the U.S. have RP.It causes retinal degeneration affecting the retina's ability to respond to light.The photoreceptor cells (rods and cones) in the eyes slowly die due to RP.
It causes slow loss of vision, beginning with decreased night vision and loss of peripheral vision eventually leading to blindness. There is no cure for RP. Only the disease progression can be slowed.
References:
- Masayo Takahashi et al. iPSC-Derived Retina Transplants Improve Vision in rd1 End-Stage Retinal-Degeneration Mice. Stem Cell Reports; (2017) doi.org/10.1016/j.stemcr.2016.12.008
- Photoreceptor Cells (Photosensitive Cells) - (https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024257/)
- Age-Related Macular Degeneration (AMD) - (https://nei.nih.gov/health/maculardegen)
- What Is Retinitis Pigmentosa? - (https://www.aao.org/eye-health/diseases/what-is-retinitis-pigmentosa)
- Retinitis Pigmentosa - (http://www.blindness.org/retinitis-pigmentosa)