- Patients from minority populations could safely get kidney transplants from deceased donors with different blood type
- Increased access to transplants and reduced waiting time is possible by expanding blood type eligibility guidelines
- New research recommends universal adoption of a policy allowing transplantation of blood type A2 organs to type B
Read More..
Kidney Transplantation in Minority Populations
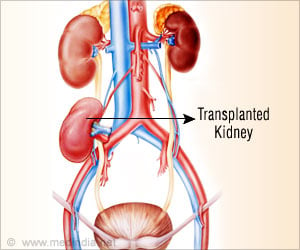
African Americans and Hispanics are at a higher risk of end-stage renal disease when compared to other ethnic or racial groups. Despite this, the availability of suitable organs has remained restricted owing to the blood type disparities. All organs, including kidneys, are allocated on the basis of blood type compatibility between donor and recipient.For example, transplantations happen only between type A blood donors and recipients, type B donor organs are slated only for type B recipients and so on. Only 20 to 25 percent of the population has type B blood; of this, the majority of individuals are African American or Hispanic. Therefore, the minority patients have always had limited access to donor’s kidneys or waited long periods of time for donor organs in contrast to Caucasians.
UNOS and Kidney Allocation System (KAS)
In order to fix the above disparity and use the available organs more effectively, the United Network for Organ Sharing (UNOS) amended the nationwide Kidney Allocation System (KAS) in December 2014. This alteration allowed for transplantation centers to offer kidneys from A2 blood type individuals to type B recipients. Around 20 percent of the population has type A2 blood, which acts as the universal donor type O.UNOS observed at the end of November 2016 that this change had led to African Americans and Hispanics receiving kidney transplants at the same rate as Caucasians.
Despite this success, the policy had not been adopted by all transplantation centers. At the end of 2017, only 18 percent of them were performing such transplants. UNOS used a survey to understand that transplantation centers had difficulty in establishing protocols to determine which type B patients were suitable for transplantation of a type A2 organ.
In this context, a research team from Vanderbilt University Medical Center, Nashville, Tennessee has attempted to evaluate long-term patient outcomes in altered blood type transplants in order to increase the availability of donor organs and reduce wait times for kidney transplantation among African American and Hispanic populations.
Study Design
The team from the Vanderbilt Medical Center established a consistent method to determine patient eligibility for transplantations between type A2 and B organs based on regular pre-transplantation blood titer measurements outlined in earlier studies.Dr. David Shaffer, Chief of Kidney and Pancreas Transplantation and lead study author observes, “The transplant community may not have been aware of these prior studies or were unsure what to do. What we found in the literature and in our study was, yes, quarterly monitoring of pre-operative anti-A titers was feasible and straightforward and identified those B recipients in whom it was safe to proceed with A2 donor transplants.”
The outcomes for 29 patients who received an A2 to B kidney transplant and 50 who received a B to B transplant were compared in the study. These patients were observed for three years and at the end, no difference was noted in the patient or graft survival at one or two years. There was no difference in renal function either.
Findings of the Study
The outcomes in minority patients who received donor kidneys that were fully immunologically compatible were similar to those who received organs from fully compatible donors. Three years following transplantation, patient and graft survival rates were the same for minorities who received a donor kidney with the same blood type as for those that received a donor kidney that carried a different blood type but had compatible immune system markers.The study, whose findings would be published in the Journal of the American College of Surgeons, is the first single-center study since the UNOS analysis in 2014, to understand the altered blood type transplants. The team hopes that the results might boost other kidney transplantation programs to expand blood type eligibility guidelines for minority patients.
The study is also the first to throw light on the follow-up required for post-transplantation titers, noticing that they do not have to be expensive. Dr. Shaffer mentioned, “Some anecdotal reports in the literature associated high post-transplant titers with graft failure, rejection, and poor overall outcomes.” He also added, “Our study is the first one to show that association is basically untrue. Titers after transplantation fluctuate widely, but even if they are high, there is no need to proceed to a biopsy or another test that would increase cost.
Cost Factor
The research team noted a significant difference in cost in these types of transplants as compared to routine transplants. Over the three-year period, pre-transplantation titer screening added more than $76,500. Total hospital costs were higher by nearly $23,000 for type B patients who received A2 organs than for patients who received a B to B organ.Dr. Shaffer explained, “This was the first study to report on the costs associated with A2 to B transplantation. One of our next steps is to look at costs over a broader period of time. We also plan to study ways of bringing down costs.” He believes that, as transplantation centers gain experience by performing these transplants, the costs may go down.
In conclusion, he remarked, “Our study shows that the UNOS policy to increase access to kidney transplantation for minorities works. Transplantation centers should consider offering this type of organ to their blood type B patients.”
Reference:
- A2 to B Kidney Transplantation in the Post-KAS Era: A 3-year Experience with Anti-A titers, Outcomes, and Costs - (https://www.journalacs.org/article/S1072-7515(19)30020-1/fulltext)
Source-Medindia