- Higher doses of radiation therapy does not increase the survival rates in prostate cancer patients.
- Patients who received higher doses of radiation experienced more side effects which sometimes manifested years after treatment.
- Higher doses should only be opted for when these doses can be safely delivered to the patient without causing adverse side effects down the line.
Study Design
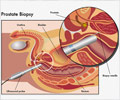
The study included nearly 1,500 patients with intermediate-risk prostate cancer. This category of patients had PSA scores of 10-20 ng/ml and a Gleason score of seven, which is a measure of tumor aggressiveness.Study findings
- Of the patients receiving standard treatment, 75% were still alive after 8 years of follow-up and among the patients who received the dose-escalation treatment, 76% were alive at the 8 year mark. The difference is not statistically significant.
- At the 8 year mark, the death rate due to prostate cancer for patients receiving standard treatment was 4% compared with 2% for patients receiving the escalating dose. The rates were also were not statistically different.
- Patients in the escalating dose group experienced more side effects such as urinary irritation or rectal bleeding, sometimes years after treatment.
Looking at the side effects of higher doses of radiation, Michalski said: "If we can safely deliver the higher dose of radiation, my opinion is to do that. It does show lower risk of recurrence, which results in better quality of life. But if we can't achieve those 'safe' radiation dose goals, we shouldn't put the patient at risk of serious side effects down the line by giving the higher dose. If we can't spare the rectum or the bladder well enough, for example, we should probably back off the radiation dose. It's important to develop treatment plans for each patient on a case-by-case basis."
Reference:
- Michalski JM, Moughan J, Purdy J, Bosch W, Bruner DW, Bahary JP, Lau H, Duclos M, Parliament M, Morton G, Hamstra D, Seider M, Lock MI, Patel M, Gay H, Vigneault E, Winter K, Sandler H. Effect of standard vs. dose-escalated radiation therapy for patients with intermediate-risk prostate cancer: The NRG Oncology RTOG 0126 randomized clinical trial. JAMA Oncology. (2018) DOI: 10.1001/jamaoncol.2018.0039
Source-Medindia