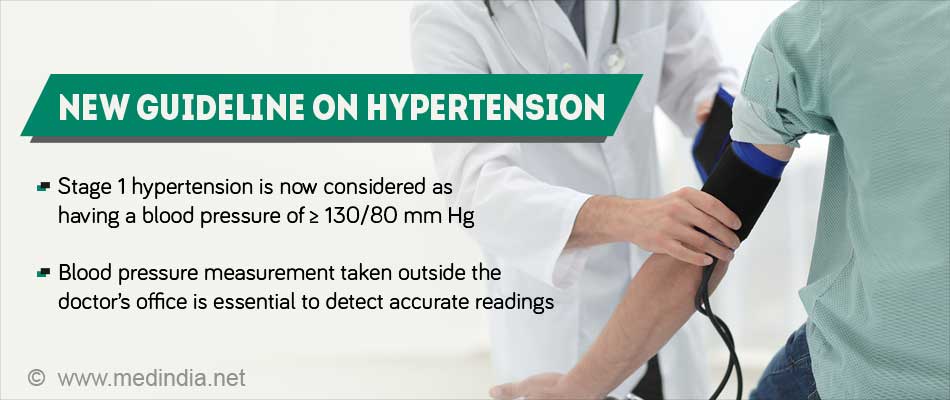
- The threshold for diagnosing hypertension in adults has been lowered from 140/80 mmHg to 130/80 mmHg
- It is very necessary to take out-of-office blood pressure to identify patients whose measurements are influenced by the atmosphere of a doctor’s office
- Implementing the new guideline will improve cardiovascular health for U.S. adults
A 21-member panel of multidisciplinary experts that included physicians, nurses, pharmacists, and patient representatives who had no BP-related industry relationships were instrumental in developing the 2017 guideline.
High blood pressure should be treated earlier with lifestyle changes and in some patients with medication – at 130/80 mm Hg rather than 140/90 - based on the new guideline. The definition of high blood pressure is lowered to account for complications that can occur at lower numbers and to allow for earlier intervention.
The new definition will result in 46 percent of the U.S. adult population having high blood pressure, with the greatest impact expected among younger people. Also, the prevalence of high blood pressure is expected to double among women less than 45, and triple among men under age 45. However, only a small increase is expected in the number of adults requiring antihypertensive medication.
"You've already doubled your risk of cardiovascular complications compared to those with a normal level of blood pressure," said Paul K. Whelton, MB, MD, MSc, FACC, lead author of the guideline. "We want to be straight with people – if you already have a doubling of risk, you need to know about it. It doesn't mean you need medication, but it's a yellow light that you need to be lowering your blood pressure, mainly with non-drug approaches."
Why did the committee move the bar down?
- First of all, people who are at the level of stage 1 hypertension are already at risk of heart attack and the committee felt that people should know that and be empowered to make a change.
- Secondly, there is enough evidence from non-drug trials and drug trials that getting down below those levels is beneficial.
Salient Features of the New Guidelines
- What your blood pressure reading means after the change
- <120/80 mm Hg - Normal Blood Pressure
- 120–129/<80 mm Hg - Elevated hypertension (pre-hypertension)
- 130–139/80–89 mm Hg (or ≥ 130/80 mm Hg) - Stage 1 hypertension
- ≥ 140/90 mm Hg - Stage 2 hypertension
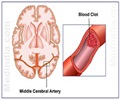
- The guideline suggests prescribing medication for adults with stage I hypertension who have existing CVD such as a heart attack or stroke, for adults with a calculated 10-year CVD risk ≥10 percent (greater than or equal to 10 percent), and for those who are at high risk based on age, presence of diabetes or renal disease; the threshold to start treatment for any of the above categories has been lowered from 140/80 mmHg to 130/80 mmHg
- The guideline stresses the importance of using the proper technique to arrive at the accurate BP reading; the reading has to be an average of ≥ 2 readings taken on ≥ 2 occasions.
- The guideline also stresses on the greater use of out-of-office readings of BP. These would include ambulatory blood pressure (ABPM) and home-based blood pressure (HBPM), especially to detect white coat hypertension (WCH) and more importantly masked hypertension (MH). The committee highlights the value of appropriate training of health care providers to tell patients about WCH.
- WCH is a condition when the BP of a person is normal or near-normal during out-of-office recordings but increases to stage 1 hypertension at the doctor’s office. On the other hand, MH is one that shows normal or near-normal at the office but increases during out-of-office recordings. WCH has a CVD risk more or less equal to a normal BP, whereas MH has a two-fold CVD risk similar to that of sustained hypertension.
- The studies that the committee analyzed indicated that for old individuals with very high systolic and low-low diastolic pressure the patients who were randomized to the lower pressure seem to do better; so they recommend that the focus should be on getting the systolic low and not worry too much about how low the diastolic goes with the medications.
- In those who might need two or more types of medications to control blood pressure, they recommend that the multiple medications be combined into a single pill so that people take their pills more consistently.
- Identifying socioeconomic status and psychosocial stress as risk factors for high blood pressure that should be considered in a patient's plan of care.
The SPRINT trial also encountered serious adverse effects in both the control and the intervention groups. To address this, Paul K. Whelton says that clinicians should be savvy and knowledgeable. When they embark on therapy, especially intensive therapy, it has to be done and monitored carefully, and if there are any adverse outcomes like symptomatic hypotension (low blood pressure) or electrolyte abnormalities, the drugs should be changed or their dose modified.
References:
- Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of the2017 American College of Cardiology/American Heart Association Hypertension Guideline Free - (http://annals.org/aim/fullarticle/2670318/prevention-detection-evaluation-management-high-blood-pressure-adults-synopsis-2017)
- ACC/AHA Hypertension Guideline: What Is New? What Do We Do? - (https://www.aafp.org/afp/2018/0315/p372.html)
- New ACC/AHA High Blood Pressure Guidelines Lower Definition ofHypertension - (https://www.acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017)
- 2017 Guideline for High Blood Pressure in Adults - (https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2017/11/09/11/41/2017-guideline-for-high-blood-pressure-in-adults)
- AAFP Decides toNot Endorse AHA/ACC Hypertension Guideline - (https://www.aafp.org/news/health-of-the-public/20171212notendorseaha-accgdlne.html)
- Katy J. L. Bell, Jenny Doust, Paul Glasziou. Incremental Benefits andHarms of the 2017 American College of Cardiology/American Heart Association High Blood Pressure Guideline. JAMA InternalMedicine, 2018; DOI: 10.1001/jamainternmed.2018.0310
Source-Medindia