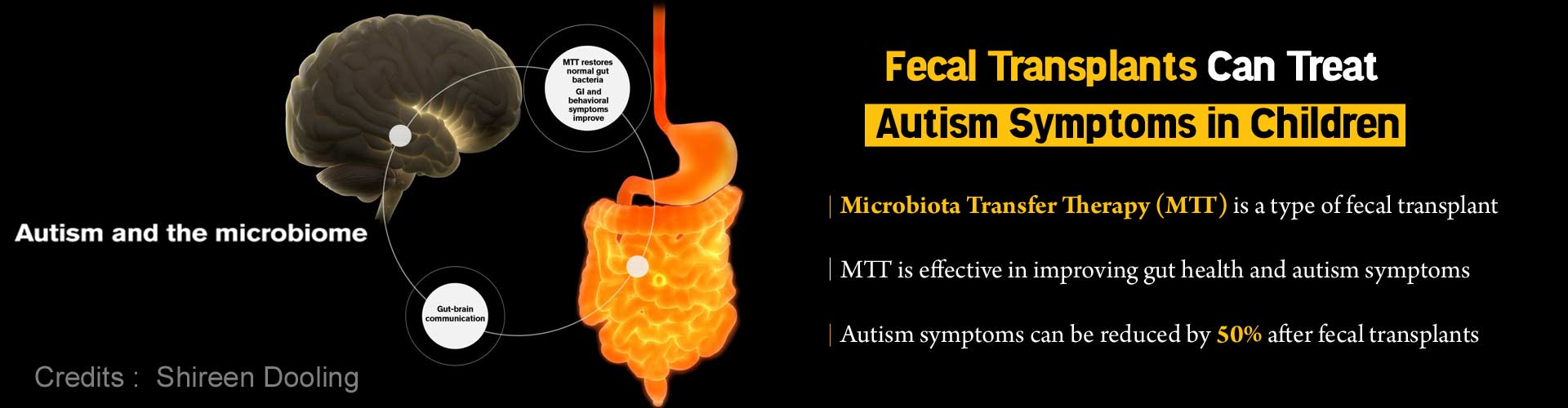
Highlights:
- Fecal transplants could treat autism symptoms in children
- Microbiota Transfer Therapy (MTT), a type of fecal transplant has been found effective in improving gut health and autism symptoms
- Larger clinical trials will be required to make this an FDA-approved treatment
Read More..
Autism – An Overview
About one in every 59 children in the U.S is diagnosed with autism presently, in contrast to one in every 150 back in the year 2000, the Centers for Disease Control and Prevention has reported. According to them, “About half a million people on the autism spectrum will become adults over the next decade, a swelling tide for which the country is unprepared.” Alongside the rise in Autism Spectrum Disorder, resistance to treating it has also been persistent. This has prompted a large number of researchers to explore the condition using novel approaches.Behavioral therapy, speech and social therapy, psychiatric medications, and dietary and nutritional approaches are the treatments currently used in treating ASD. Nonetheless, there are no approved medical treatments available for treating the core symptoms of ASD which include difficulty in social communication and repetitive behaviors.
Microbiota Transfer Therapy (MTT)
MTT, a special type of fecal transplant, initially pioneered by Dr. Thomas Borody, an Australian gastroenterologist has been highly beneficial in treating children diagnosed with ASD in the long term. Autism symptoms and gut health have improved and the improvements have also persisted in the long term after the treatment, which is significant.A research angle involving the gut microbiome appears very promising in treating ASD. Gut microbiome is the collection of microbes in the intestines that helps in digestion, training the immune system and preventing excessive growth of harmful bacteria. The gut microbiomes also affect brain communication and neurological health, recent research hints. There is growing interest worldwide about the notion that changes in normal gut microbiota could be accounted for triggering a wide range of diseases.
The research team from Arizona State University, Rosa Krajmalnik-Brown, James Adams, Dae-Wook Kang – also the lead author, have demonstrated the benefits of the Microbiota Transfer Therapy (MTT) in a new study. The study, “Long-term benefit of Microbiota Transfer Therapy in Autism Symptoms and Gut Microbiota,” has been published in the Scientific Reports.
Learnings from the Study
Most of the initial improvements in gut symptoms continued to remain even after two years post-treatment. A steady reduction of ASD symptoms during the treatment and over the next two years were reported by the parents as well. A 45 percent reduction in the core symptoms of ASD was noted by a professional evaluator at two years post-treatment as compared to when the treatment began.“We are finding a very strong connection between the microbes that live in our intestines and signals that travel to the brain,” said Krajmalnik-Brown, Professor, Biodesign Swette Center for Environmental Biotechnology at the Biodesign Institute and ASU's School for Sustainable Engineering and the Built Environment. “Two years later, the children are doing even better, which is amazing,” she added.
On the association between autism and gastrointestinal (GI) problems, Krajmalnik-Brown said, “Many kids with autism have gastrointestinal problems, and some studies, including ours, have found that those children also have worse autism-related symptoms. In many cases, when you are able to treat those gastrointestinal problems, their behavior improves.”
Around 30-50 percent of people with autism have chronic gastrointestinal (GI) problems, mostly constipation and diarrhea or either, that can last for several years. This will result in continuous discomfort and pain which in turn could lead to irritability, decreased attention and learning, and negatively impact behavior as well.
An earlier study had found temporary improvements in GI and autism symptoms when just an antibiotic, Vancomycin was used. The benefits were only short term despite continued use of over-the-counter probiotics.
The research team was faced with the question of what's going on in the gut, how does it affect both physical and behavioral symptoms of autism, and how a long-lasting treatment could be developed. The work of Krajmalnik-Brown, Kang and Adams has exhibited that it is possible to ‘donate’ a more diverse set of bacteria into the patient and improve gut health by transferring healthy microbiota to individuals missing specific gut bacteria.
Thomas Borody’s Contribution to the Study
Fecal Microbiota Transplantation (FMT) was initially developed by Professor Thomas Borody in Australia. He has overseen close to 18,000 FMTs for various illnesses at the Centre for Digestive Diseases in Sydney since 1987. In Australia, he established the use of FMT for colitis and Clostridium difficile infection, and was also the first to use oral FMT to treat children with ASD.Though a single dose of FMT was typically sufficient to treat C. Difficile infections, this was not enough for Borody’s patients with autism who were far harder to treat. They required FMT every day for three months and eventually, there were significant improvements in both GI and autism symptoms.
Borody used this experience to lead the design of the clinical treatment used for this study at ASU. Pre-treatment with Vancomycin, a bowel cleanse, a stomach acid suppressant, and fecal microbiota transfer daily for seven to eight weeks were all part of the 10-week MTT approach.
Study Design
“This exploratory, extended-duration treatment protocol thus appears to be a promising approach to alter the gut microbiome and improve GI and behavioral symptoms of ASD. Improvements in GI symptoms, ASD symptoms, and the microbiome all persisted for at least eight weeks after treatment ended, suggesting a long-term impact,” concluded an initial open-label study led by Krajmalnik-Brown and Adams, published in the journal Microbiome in 2017. Whereas the present study shows that the benefits persisted at least two years post-treatment.The microbiome of children with autism was compared to those in typically developing children by the ASU team and differences were noted. Low diversity in gut microbes and depletion of certain strains of helpful bacteria, such as Bifidobacteria and Prevotella were found in children with autism at the start of the study.
“Kids with autism are lacking important beneficial bacteria, and have fewer options in the bacterial menu of important functions that bacteria provide to the gut than typically developing kids,” said Krajmalnik-Brown.
Microbial diversity as well as the presence of Bifidobacteria and Prevotella, the helpful bacteria in the gut, significantly increased following the FMT treatment; diversity was higher and the beneficial microbes continued to be present even after two years.
“We originally hypothesized that our therapy would be efficient to transform the dysbiotic gut microbiome toward a healthy one. In our original paper in 2017, we reported an increase in gut diversity together with beneficial bacteria after MTT, and after two years, we observed diversity was even higher and the presence of beneficial microbes remained,” said Kang. While this may be one of the reasons behind the success of the improved gut health, additional mechanistic studies would be required to define specific roles of gut microbes in the context of autism, he added.
Effectiveness of the Treatment
The work done at ASU goes beyond merely treating patients, also focusing on developing better formulations and optimize dosing based on knowledge gained from the treatment.“Understanding which microbes and chemicals produced by the microbes are driving these behavioral changes is at the heart of our work,” Krajmalnik-Brown said. The study demonstrated that two years after treatment stopped the participants still had an average of a 58 percent reduction in GI symptoms compared to baseline. Additionally, the parents of most participants reported ‘a slow but steady improvement in core ASD symptoms,’ the team's new publication reported.
Speaking about the dedication of the families to the research, Adams said, “Every family completed the study, and every family returned two years later for a follow-up evaluation.” “The treatment was generally well-tolerated with minimal adverse effects,” he added.
Commenting on the study’s achievement, Borody said, “This is a world-first discovery that when we treated the gut bacteria in these children during our clinical trial two years ago to reset their microbiome with FMT, positive results are still continuing to be improving two years from the original treatments. I would call it the highest improvement in a cohort that anyone has achieved for autism symptoms.”
Significant Findings from the Study
When compared to the baseline, there was a 45 percent decrease in ASD symptoms, professional evaluations revealed. Though there may be some placebo effect, most of the effect appeared to be real, the team observed. While 83 percent of the participants were rated as having ‘severe’ autism when the study began, only 17 percent were ‘severe,’ 39 percent ‘mild/moderate’ and 44 percent below the cut-off for mild ASD, at the end of it.Greg Caporaso, a co-author on these studies, and a leading expert in microbiome data science from Northern Arizona University helped in analyzing the microbiome data to better understand bacterial changes as a result of MTT.
“Drs. Krajmalnik-Brown, Kang and I are excited about the results, but we want to caution the public that we need larger clinical trials for this to become an FDA-approved treatment,” said Adams. Safe and effective treatment requires professional expertise. The GI distress is improved by the MTT technique by introducing key strains of beneficial bacteria and helping in raising the levels of biodiversity within the gut, boosting health overall in turn.
The Research Team
Dr. James Adams, whose daughter was diagnosed with autism, had both professional and personal reasons to pursue ways to help children with autism because of his first-hand knowledge of the situation. He is a President's Professor at the School for Engineering of Matter, Transport and Energy and also the programme chair of Materials Sciences at ASU. Adams is also the President of the Autism Society of Greater Phoenix, one of the biggest parent support groups in Arizona.“Dr. James Adams is the reason why I started working on autism,” said Krajmalnik-Brown.
“I had the methods to do all of the measurements and assessments in the microbiome part of the work, and he had the autism knowledge,” she added.
Patient recruitment, supervising clinical work and ASD assessments and guiding the patients through the trials were handled by Adams and the microbiome evaluations and plan of the study were done by Krajmalnik-Brown.
Other Observations
All the study participants exhibited chronic GI symptoms including chronic constipation and/or chronic diarrhea from infancy. Certain parents noted that their children's behavior had improved over time, extending the benefits of the treatment beyond just physical improvements.“It is very unusual to see steady gradual improvement after the conclusion of any treatment. We only conducted the long-term follow-up study after several families told us that their child was continuing to improve significantly,” remarked Adams .
The study data suggests that MTT treatment technique made the gut environment healthier, thereby improving both the GI and ASD symptoms long term, Krajmalnik-Brown stated.
Way Forward
Birth via C-section, reduced breastfeeding, higher intake of antibiotics, and decreased fiber intake by mothers and their children were some of the common traits shared by the trial participants, all of which lead to limited biodiversity in their gut bacteria, Adams mentioned. The small sample size and the open-label nature of the study, call for more research in order to validate if the MTT technique could be therapeutic.The optimal dose and treatment duration followed were ‘first generation’ estimates in the initial study and were sufficient to substantially benefit 90 percent of the children. The team is currently working on optimizing the dosing and treatment duration in order to improve the benefits further and to ascertain if booster doses may be required in some cases.
References:
- Autism symptoms reduced nearly 50% two years after fecal transplant - (https://biodesign.asu.edu/news/autism-symptoms-reduced-nearly-50-two-years-after-fecal-transplant)
Source-Medindia