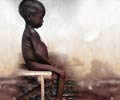
Good healthy nutrition is vital for every child’s growth and development. However, it is estimated that globally about 55 million children under the age of 5 years suffer from severe acute malnutrition (SAM). Malnutrition is responsible for an alarming 35% of deaths among children under 5 years.
WHO recommends mid-upper-arm circumference (MUAC) or weight-for-height Z-scores (WHZ) for assessment of acute malnutrition. Severe acute malnutrition is defined by a very low weight for height (less than -3z score or a mid-upper-arm circumference less than 115 mm) or the presence of bilateral pitting edema by World Health Organization (WHO).A systematic review of the evidence was conducted so as to assess the validity of these observations and compare the degree of discrepancy between countries. The choice of the anthropometric indicator for monitoring nutritional rehabilitation and deciding discharge was also evaluated.
Different databases such as Medline, Cochrane Library, CRD database, Embase amongst others were searched and evaluated to check for any evidence of adverse events, treatment duration, costs and mortality when the SAM children were admitted to and discharged from hospital based on MUAC as stand-alone criteria compared to using WHZ.
It was noted that out of the eleven studies which were included, only one cohort study compared children with an MUAC < 115 mm and those with WHZ <-3 at the start of the rehabilitation period.
Four studies reportedly admitted SAM children based on only MUAC values. The mortality risk was relatively low in three studies and was reported to be £2.1%.
One study reported a lower daily MUAC gain especially in younger and smaller children and in females. Two studies discharged children on the basis of MUAC (MUAC ≥124 mm only or MUAC ≥130 mm), but did not conduct any follow-up after discharge.
It was seen that none of the studies conducted any follow-up of children after discharge to check for any risk of relapse or longer-term mortality.
The findings of this evaluation suggest that MUAC could be used adequately as a stand-alone criterion for the diagnosis, monitoring and discharge of SAM children. However, a strong recommendation could not be made for the same due to lack of sufficient and conclusive evidence. In addition, factors such as age, sex and stunting should also be taken into consideration and see if they have any effect on the rehabilitation outcomes.
References:
1. http://www.who.int/nutrition/publications/guidelines/updates_management_SAM_infantandchildren_review1.pdf
2. http://www.actionagainsthunger.org/sites/default/files/publications/Acute_Malnutrition_A_Preventable_Pandemic_01.2009.pdf
Source-Medindia