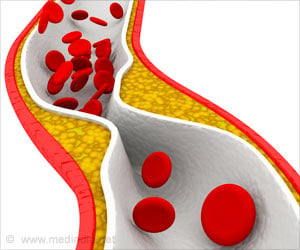
- Treatment of atherosclerotic vessel disease with drugs (eg: statins) that lower cholesterol levels alone may not be sufficient to prevent heart attacks.
- Current study shows that addressing an immune reaction that turns on the signal for reducing blood vessel inflammation can regress atherosclerotic plaques and reverse disease.
Are Current Treatments For Atherosclerosis Really Satisfactory?
During the course of one’s life, cholesterol, more specifically LDL or bad cholesterol gets deposited in the wall of blood vessels. By the time a person reaches his 4th decade, these deposits have evolved into inflamed plaques (due to a chronic reaction to cholesterol), and if severe, can dislodge and block the vessel and cause serious conditions like heart attacks and strokes. "Even the latest, most potent cholesterol-lowering drugs, PCSK9 inhibitors, let alone widely used statins, cannot fully reverse damage done to arteries over time, and so they can't prevent roughly 500,000 heart attacks per year in the United States," says lead study author Edward Fisher, MD, PhD, director of the Marc and Ruti Bell Vascular Biology and Disease Program at NYU Langone.With a view to this goal, the research team analyzed the molecular events that took place in atherosclerotic vessels where the plaques underwent either progression or regression.
Molecular Events In The Atherosclerotic Vessel – Details Of The Study
The study team conducted their study in mice and made the following observations.- The LDL cholesterol deposited in the vessel wall triggers the inflammatory pathway that normally attacks invading microbes or foreign antigens.
- Blood cells called monocytes are stimulated and reach the site of cholesterol deposition in the blood vessel.
- In conditions where the plaques worsened, proinflammatory signals that caused the monocytes to become proinflammatory M1 macrophages were switched on, leading to progression of the plaque and cause complications such as plaque rupture.
- In situations where the plaques were regressing, anti-inflammatory signals dampened inflammation that caused healing and reversal of the plaque.
- When mice were genetically modified to prevent monocytes from becoming M2 macrophages, it was not possible for them to achieve normal disease regression.
- When plaques from diseased mice were transplanted into the arteries of healthy mice, there was a dramatic drop in cholesterol levels. This drop also stimulated a second benefit in mice, where monocytes automatically became M2 instead of M1 macrophages followed by rapid plaque regression.
Scope Of Current Research, Cues From Earlier Research And Future Research Plans
The current study has established that plaque regression can occur with reversal of atherosclerotic disease. Future research projects are needed to validate their observations and gain more insight into the underlying mechanisms include the following.- Newer imaging studies may be necessary to visualize the plaque and determine the number and type of macrophages.
- The local signals in the blood vessels that turn on the M1 or M2 switch must be identified and established. Among the prominent candidates are the signaling proteins interleukin-4 (IL-4) and interleukin-13 (IL-13), which have been shown in prior research to be associated with the M2 pathway.
- Earlier research has shown that the IL-4 and IL-13 turn on the STAT6 (signal transducer and activator of transcription 6) pathway which directs the monocyte to become an M2 macrophage. Blocking this pathway reduced the number of M2 macrophages in the regressing plaque.
- Drugs that boost monocyte to M2 macrophage conversion may be a therapeutic option to reduce heart attacks or strokes.
- The Fisher team is testing out nanoparticles based on the structure of HDL or good cholesterol. They are also testing nanoparticles that are programmed to deliver IL-4 into the plaque.
- They will next plan nanoparticle based studies in pig models which could set the stage for human trials.
Source-Medindia