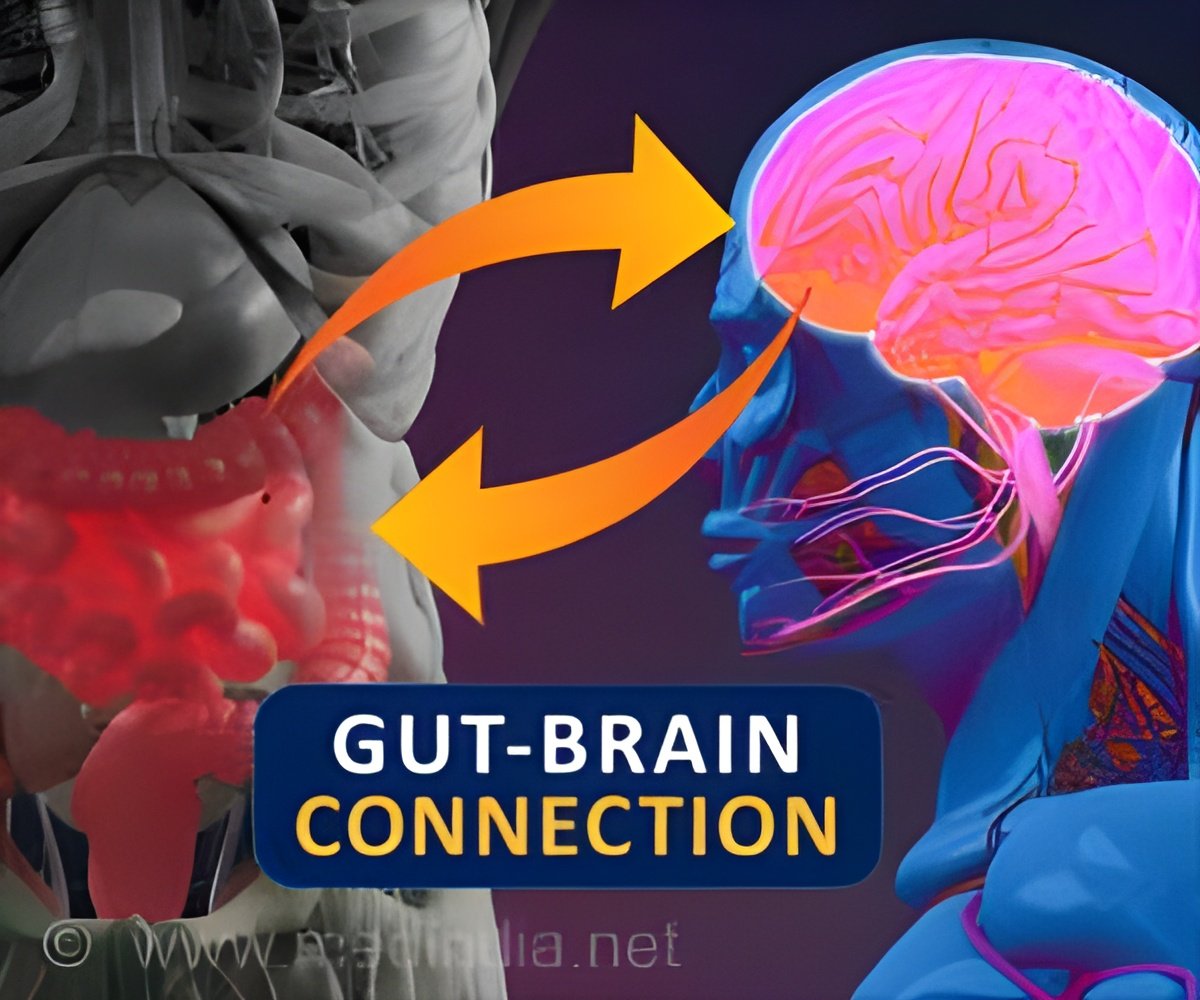
Gut-Brain Connection: Bacteria in the gut may influence brain structure and clinical symptom severity in heavy drinkers.
The gut-brain axis in individuals with alcohol use disorder: An exploratory study of associations among clinical symptoms, brain morphometry, and the gut microbiome
Go to source).
‘Did You Know?
Your gut bacteria can influence brain function and behavior. #GutBrainConnection #Alcoholconsumption #AlcoholUsedisorder’





Your gut bacteria can influence brain function and behavior. #GutBrainConnection #Alcoholconsumption #AlcoholUsedisorder’
Discovering the Gut-Brain Connection
The human gut microbiome refers to bacteria that live within humans and perform vital physiologic functions such as immune regulation and nutrient metabolism. Heavy alcohol consumption has been linked to changes in this microbiome, including decreases in certain helpful bacteria, reduced microbial diversity, and increases in inflammatory bacteria. Recent research also suggests certain bacteria in the gut microbiome can influence brain function and behavior and may be associated with the development of psychiatric disorders such as alcohol use disorder.This exploratory secondary analysis categorized the gut microbiome by quantifying the abundance of bacteria and inferred functional potential using gut-brain modules: neuroactive signaling pathways informed by the literature and calculated from genes annotated in shotgun metagenomics sequencing. Gut microbiome bacteria and gut-brain module abundance were compared to clinical symptom severity and the size of brain regions associated with stress signaling in people with alcohol use disorder. Although these findings are preliminary, there were patterns of bacteria that displayed clinically and statistically significant associations with the brain and symptom presentation.
The amygdala had the strongest and most consistent relationships with the gut microbiome, with researchers finding significant associations between amygdala volume and the quantity of certain types of bacteria and the diversity of bacteria in the microbiome. Greater amygdala volume was associated with increases in some types of bacteria and decreases in other types of bacteria, including bacteria associated with toxins entering the bloodstream, and is associated with inflammation in end-stage organ disease in people with alcohol use disorder. Amygdala volume was negatively associated with GABA synthesis pathways and positively associated with glutamate synthesis pathways, which are involved in modulating signaling related to symptoms such as withdrawal and anxiety.
Different bacterial species classified to the genus Blautia were negatively associated with amygdala volume but positively associated with severity of symptoms such as depression or sleep quality. The prevalence of Escherichia coli bacteria in gut microbiome samples was negatively associated with amygdala volume and positively associated with craving for alcohol. Higher Prevotella copri in the gut microbiome samples was associated with lower self-reported symptoms of anxiety, depression, and sleep quality.
The study is limited by the small sample, which included 16 participants with alcohol use disorder in inpatient treatment, and the lack of a control group. Further research is needed to understand whether the identified differences in the gut microbiome may increase the risk for or be a result of alcohol use disorder.
Advertisement
- The gut-brain axis in individuals with alcohol use disorder: An exploratory study of associations among clinical symptoms, brain morphometry, and the gut microbiome - (https://onlinelibrary.wiley.com/doi/10.1111/acer.15346)
Source-Newswise