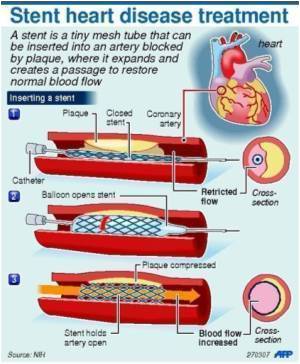
Study of many percutaneous coronary intervention procedures imply that employing drug-eluting stents differ among U.S. physicians plus only modestly correlated with the patient's risk of renarrowing.

Amit P. Amin, M.D., M.Sc., of Barnes Jewish Hospital, Washington University School of Medicine, St. Louis, Mo., and colleagues analyzed more than 1.5 million PCI procedures in the National Cardiovascular Data Registry (NCDR) CathPCI registry from 2004 through much of 2010. They sought to examine variation in DES use among physicians, whether predicted TVR risk with bare-metal stents was associated with DES use, and what the estimated clinical and economic consequences were of lower DES use among patients with low TVR risk.
"The present study demonstrates that in current U.S. practice, DES use is prevalent, even among patients at low risk of developing restenosis. There was also significant variation in the rate of DES use by individual physicians. A reduction in DES use among patients at low risk for restenosis was projected to be associated with substantial costs savings with only a small increase in TVR events," the authors note.
According to study results, drug-eluting stent use was 73.9 percent among those at a low risk for TVR, 78 percent among those at moderate risk and 83.2 percent among those at the highest TVR risk.
The study suggests that a 50 percent reduction in the use of DES in low-TVR-risk patients was projected to lower health care costs by about $205 million per year in the U.S., while increasing the overall TVR event rate by 0.5 percent.
"Given the marked variation in physicians' DES use, a strategy of lower DES use among patients at low risk of TVR could present an important opportunity to reduce health care expenditures while preserving the vast majority of their clinical benefit," the authors conclude.
Advertisement
Invited Commentary: Our Health System's Flawed Relationship with Technology
Advertisement
"The use pattern of DES during the past nine years illustrates how far away the system is from consistently embracing value-based medical decision making, and it also enumerates the many barriers and inertial practices in U.S. health care that must be surmounted to reach economic sustainability," Groeneveld concludes.
Source-Eurekalert