"These results are just one example of how our best science can advance the treatment of an important disease, TB, that exacts a huge toll among HIV-infected individuals," says NIAID Director Anthony S. Fauci, M.D. "With an estimated 1.4 million HIV-infected individuals developing TB in 2008 alone, we must continue to pursue 21st-century solutions to the scourge of HIV-TB co-infection, as well as other diseases that afflict HIV-infected people."
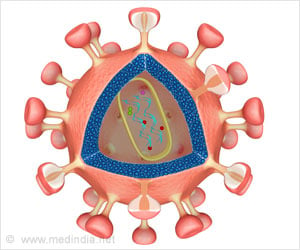
Individuals with HIV-TB co-infection in resource-limited countries frequently come to the attention of healthcare professionals for the first time when HIV already has severely damaged their immune systems. Such people often die during the first few months after beginning TB treatment. Clinicians agree that starting anti-HIV therapy during that short window can stave off death for some patients, but data on the best time to start have proven inconclusive and opinions have varied. The dilemma is that starting anti-HIV therapy before the TB infection is under control can cause the patient to become very sick and even die from a condition known as Immune Reconstitution Inflammatory Syndrome, but starting anti-HIV therapy too late may allow the patient to die from HIV infection. TB accounted for nearly a quarter of HIV-related deaths worldwide in 2008.
The clinical trial, called the Cambodian Early versus Late Introduction of Antiretroviral Drugs (CAMELIA), or ANRS 1295, launched in January 2006 at five sites in Cambodia, a country with a high prevalence of TB and HIV. The study staff enrolled 661 volunteers ages 18 and older with newly diagnosed HIV-TB co-infection and very weak immune systems (measured as fewer than 200 CD4+ T cells per cubic millimeter of blood). The participants all began receiving treatment for TB and were assigned at random to begin antiretroviral therapy for HIV either two weeks later or eight weeks later. The volunteers received powerful antiretroviral drug cocktails known as highly active antiretroviral therapy, or HAART. Study staff followed the participants for 50 weeks after the last volunteer had enrolled in the trial, performing clinical exams and biological tests at frequent intervals to monitor participants' health and safety.
By the end of the follow-up period, 59 out of 332 participants who had started HAART two weeks after beginning TB treatment had died, while 90 out of 329 participants who started HAART eight weeks after beginning TB treatment had died. This 33 percent difference was statistically significant, leading the principal investigators to conclude that starting HAART two weeks after beginning TB treatment, rather than waiting eight weeks, boosts the chance of survival for people with HIV-TB co-infection and severely damaged immune systems.
Advertisement