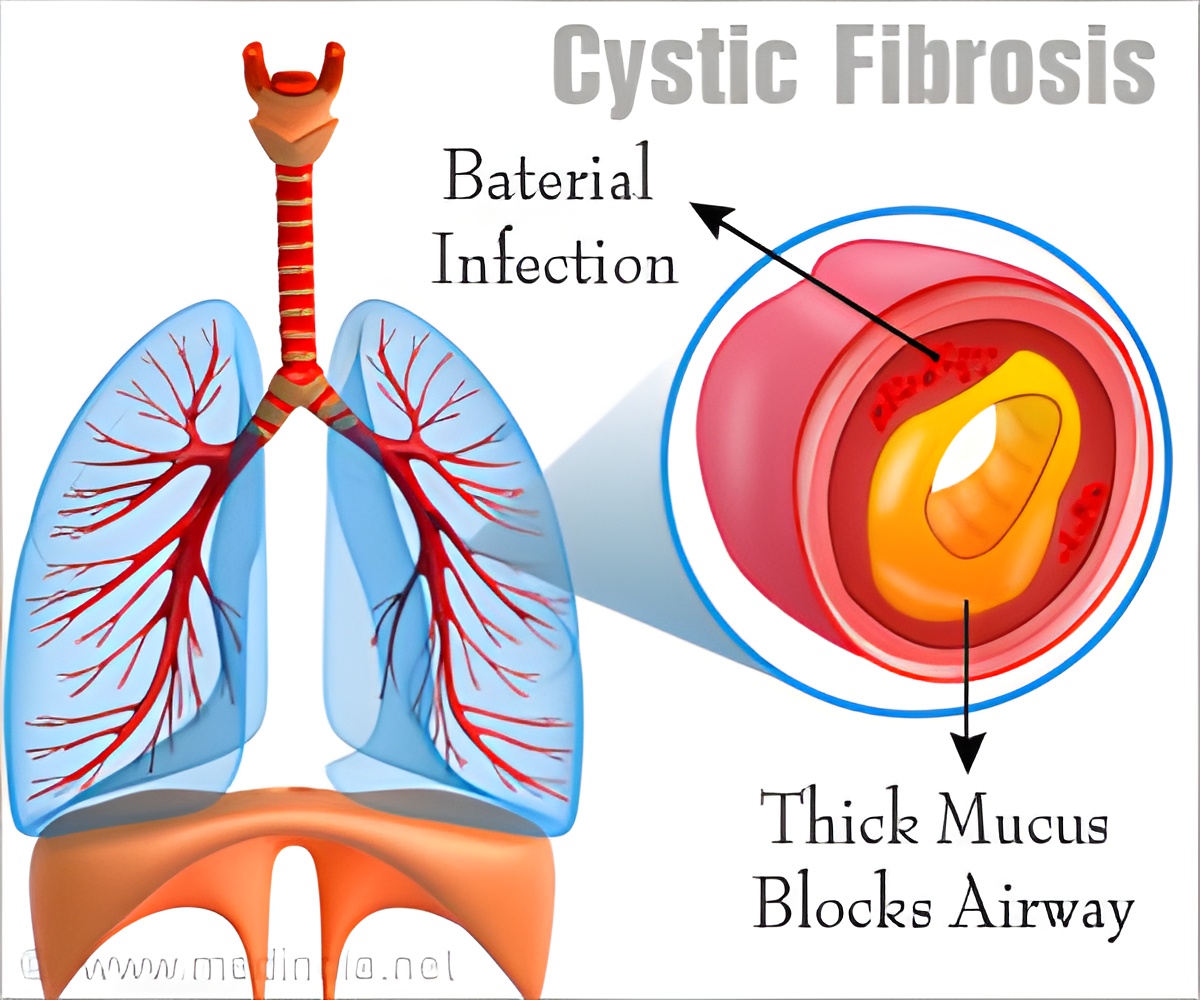
‘MgtE, a protein in the membrane of bacteria, tells the bacteria when and where to form biofilms to evade CF patient's immune system.’
Tweet it Now
MgtE activity in P. aeruginosa appears to be influenced by the bacterium's chemical surroundings, including the abnormal mucus in CF patients. Specifically, MgtE responds to fluctuations in magnesium levels. "We know quite a lot about the regulatory signaling that is involved in the bacterium telling itself to form a biofilm, but we haven't had much knowledge about the molecular signals that tell these organisms that it's an appropriate time and place to cluster," said Anderson, corresponding author of the new study. "Specifically, we haven't known what signals bacteria are receiving from the environment -- in this case, the mucus in CF patients' lungs -- to tell them to form biofilms.
"We have now tied MgtE, a protein in the membrane of bacteria, with known biofilm signaling networks. I think this is one of the first times such a link between an external signal and biofilm regulation has been identified. We are adding to the body of knowledge of biofilm formation with the ultimate goal of finding better ways to disrupt that formation, leading to improved treatments for the chronic pneumonia in CF patients."
Infections in cystic fibrosis patients cause breathing difficulties resulting in serious strain on the lungs, cardiovascular system and heart.
Advertisement