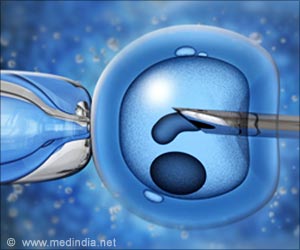
During in-vitro fertilization, using computer-automated, time‐lapse photography of embryos in the laboratory may improve embryo selection, potentially increasing the chances of pregnancy among women undergoing the procedure.

The researchers at Penn and their collaborators used the Early Embryo Viability Assessment imaging device (or Eeva, developed and manufactured by Auxogyn, Inc.), which records images of developing embryos during the first three days of laboratory culture, to evaluate embryos transferred into the uterine cavity of 177 patients. The testing process involved fitting the devices into a standard incubator and using dark field imaging to capture high resolution, single-plane pictures of embryos housed in a petri dish, at five-minute intervals. The images were then fed into a software program that uses several measures to assess the embryo's developmental potential – rating them high, medium, or low for their capacity to reach the blastocyst stage by the fifth or sixth day of culture. Embryos normally implant at the blastocyst stage – when they have divided into about 100-200 cells – and it is and it is known that blastocysts have a much greater chance of implanting successfully and resulting in an ongoing, viable pregnancy.
Information on the embryo quality rating was not available to clinicians during the IVF procedures that were part of the study, but when researchers unblinded the study results, they found that patients with at least one "high" rated embryo transferred had a 54 percent viable pregnancy rate compared to a 34 percent rate for those following transfer of only a "low" rated embryo.
"Our findings provide promising news for couples using or considering in-vitro fertilization because it shows that this technology offers the prospect of selecting embryos that have a greater likelihood of resulting in a pregnancy," said lead author Matthew VerMilyea, PhD, who was serving as director of Assisted Reproductive Technologies and Andrology Laboratories at Penn at the time of the study and is currently a consultant to the division of Reproductive Endocrinology at Penn Medicine. "What's particularly important is that our participants are from multiple clinics, each with distinctive protocols and patient populations, indicating that this technology may be generalizable and could have a significant impact in widely different laboratory settings."
After an egg has been fertilized by a sperm, normal embryos follow clear-cut timeframes for development, such as the time it takes for a two-cell embryo to turn into a three-cell embryo, and the time it takes for a three-cell embryo to turn into a four-cell embryo. Based on these patterns, computer-automated programs have the potential to predict by day two of embryo development which embryo(s) are more likely to become viable blastocysts and, as suggested by the current Penn study, result in a viable pregnancy. By using non-invasive cell tracking and prediction software, the development of each embryo is automatically analyzed against the well-validated cell division time periods. If the timing and duration of cellular divisions fall within the defined optimal time periods, an embryo is given a high probability rating for becoming a blastocyst. If division timing falls outside of the optimal time range, an embryo is given a low probability rating. The current study extends these findings by showing that embryos receiving a high rating for becoming a blastocyst, also have a higher probability to implant and result in a viable pregnancy.
At present, fertility experts examine embryos under a microscope, looking at potential indicators of health of the embryo such as the number and symmetry of cells, and degrees of cell fragmentation. Based on these assessments and following recommendations developed through observational and correlative studies, clinicians and their embryology colleagues then choose which embryo(s) to transfer to the womb. The time-lapse system used in the new study uses objective visual evidence and automated predictive algorithms to enhance this conventional approach.
Advertisement
Source-Eurekalert