‘The use of certain traditional chemotherapy drugs may expand the number of tumors that respond to immune checkpoint blockade, one of the most promising cancer therapies.’
Tweet it Now
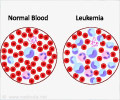
One of the ways that tumors evade the immune system is by activating immune checkpoints - molecules that normally function to suppress the activity of CTLs. While clinical trials of drugs that block immune checkpoints have induced long-term control of several types of cancer, they have done so in only a minority of patients. The reason for this selective response is unclear, but evidence has suggested that patients whose tumors already contain CTLs are more likely to benefit. The MGH-based team tested combinations of several FDA-approved chemotherapy drugs with the goal to find some that induce CTL infiltration within the tumors of several lung cancer mouse models. Only the combination of oxaliplatin and cyclophosphamide (Oxa-Cyc) did so. The researchers then showed that lung tumors in mice treated with Oxa-Cyc alone grew more slowly. Tumor control required not only CTL infiltration into tumors but also an increased activity of the innate immune system within the tumor microenvironment, which also was stimulated by Oxa-Cyc treatment. Furthermore, combining Oxa-Cyc treatment with immune checkpoint blockade durably controlled tumor growth in the lung cancer mouse models, which neither treatment was able to do alone. The investigators also identified other chemotherapy drugs that, when combined with immune checkpoint therapies in mice, could delay progression of other cancer types, including fibrosarcoma and colon cancer.
Pittet said, "The genetic mouse model of lung cancer used in this study is notoriously resistant to today's cancer treatments, in contrast to many other models that are sensitive to several chemotherapy agents. We hope this model replicates treatment-resistant disease enough so that our findings can be translated to patients, but clinical trials are needed to examine whether that will be the case. Since the drugs shown to work in this study are all FDA-approved, the combination could be quickly tested in patients with lung cancer. We also plan to explore whether precision medicine approaches, which could identify drugs that best promote tumor infiltration by CTLs in a given patient, could extend the benefits of checkpoint blockade to even more patients."
Source-Eurekalert