Can cell therapy help heart failure? Yes, it reduced the risk of heart attack and stroke and improves the heart ejection fraction of heart failure patients.
‘The effect of the cell therapy was synergistic with and additive to state-of-the-art heart failure medications’





Patients in the trial were on full guideline-recommended drug therapy for heart failure, suggesting that the effect of the cell therapy was synergistic with and additive to state-of-the-art heart failure medications. The findings are published in the Journal of the American College of Cardiology.More than 6 million Americans have chronic heart failure, a progressive disease that leads to a weakening of the heart muscle and a loss of its pumping function. Most heart failure drugs address the detrimental changes that occur in the heart as a result of pathways that are activated during heart failure to compensate for poor heart function.
These activated pathways eventually contribute to the progression of heart failure and repeated hospitalizations. Despite advances in therapies targeting these pathways, mortality rates remain high. The unique mechanism of action of MPC appears to provide an alternative approach that has the potential to make a significant impact on the high mortality of this disease.
Successful New Chronic Heart Failure Treatment Using Cell Therapy
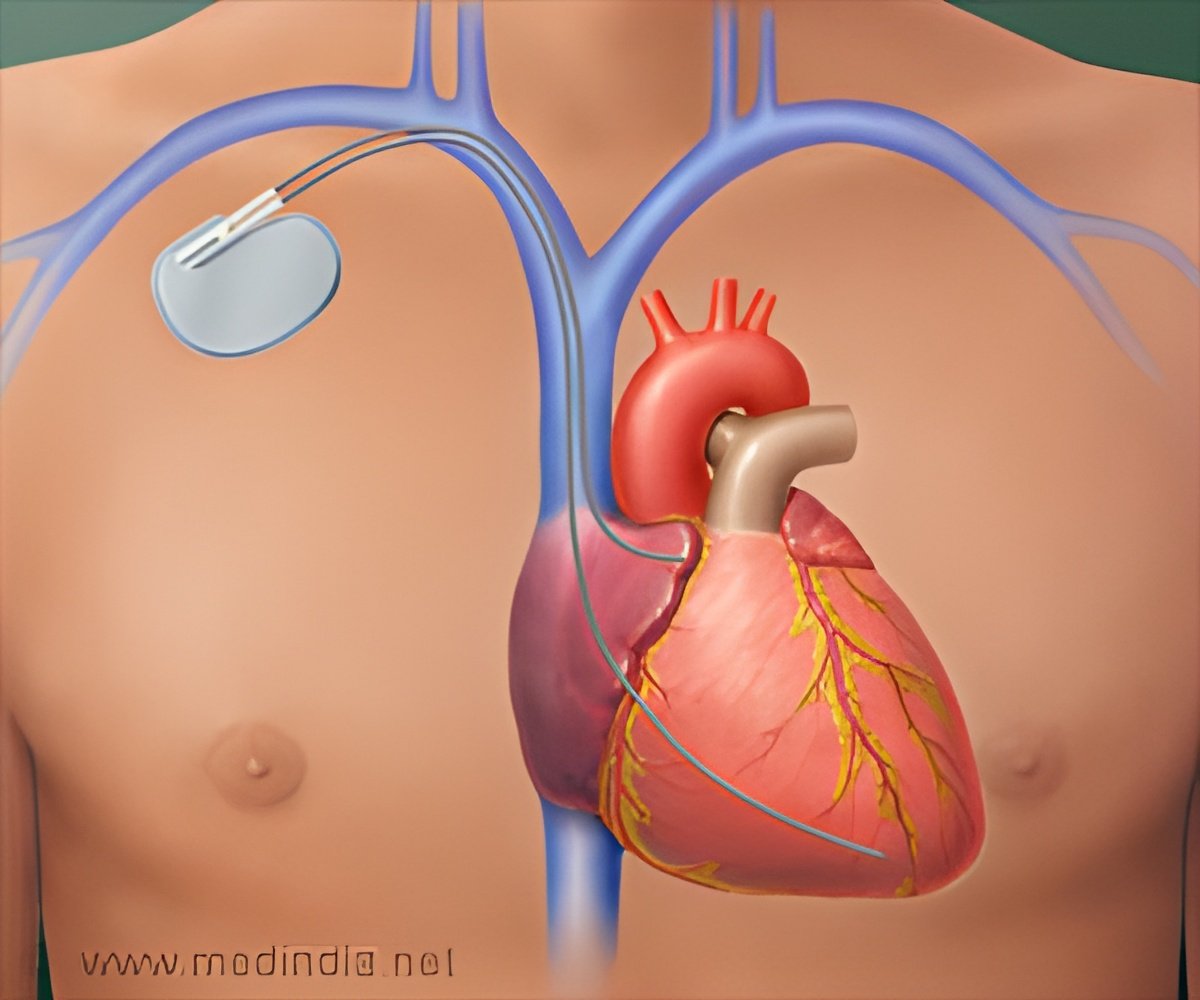
This trial was performed at 51 sites in 565 patients with chronic heart failure, who were also on standard-of-care heart failure treatment. The study, which had a mean follow-up of 30 months, was designed to examine the effects of MPC comprising immunoselected, culture-expanded mesenchymal precursor cells (MPCs), on the number of hospitalizations and major adverse cardiovascular events in heart failure.MPCs are a good candidate for use in heart failure with low ejection fraction because they have potent anti-inflammatory, pro-angiogenic, and pro-healing effects. The cells were obtained from the bone marrow of healthy adult donors. Cell-treated patients in the study received direct cardiac injections of MPCs, and control patients underwent a “sham” or mock procedure with no injections.
MPC-treated patients showed a significant strengthening of the left ventricular muscle within the first 12 months as measured by an increase in left ventricular ejection fraction, which measures the heart’s pumping ability and is one of the metrics used to assess overall heart function.
Advertisement
Similarly, to what was seen with these major adverse cardiovascular events, improvement in ejection fraction was even more pronounced in patients with higher inflammation levels.
Advertisement
Current Status of Stem Cell Therapy in Heart Failure
The results are an important step in understanding how cell therapy provides benefits in patients with chronic heart failure due to poor pump function. The cells appear to work by reducing inflammation, increasing microvascular flow, and strengthening the heart muscle.Locally, in the heart, the MPCs can protect cardiac muscle cells from dying and can improve blood flow and energetics. In large blood vessels throughout the body, the reduced inflammation resulting from the activation of MPCs may decrease plaque instability, which is what leads to heart attacks and stroke.
The findings of long-term improvements in outcomes for patients with chronic heart failure due to low ejection fraction and poor pump function are important milestones in the field of cell therapy for cardiovascular disease.
The results help in identifying those heart failure patients with inflammation who are at greatest risk and most likely to benefit from MPC therapy and findings will be confirmed in future studies. This seminal trial sets the stage for eventually adding cell therapy to the treatment arsenal for heart failure.
For millions of people in the United States over the age of 20 who suffer from heart failure, MPC therapy could change the future of cardiovascular care for patients with heart failure due to inflammation.
Source-Eurekalert















