Research has indicated that heart failure affects roughly six million Americans, yet treatment consists of either a heart transplant or the insertion of mechanical devices that assist the heart.
Dr. Bolli is conducting the groundbreaking study, "Cardiac Stem Cell Infusion in Patients with Ischemic cardiOmyopathy (SCIPIO)," in which researchers at the University of Louisville's Jewish Hospital are collaborating with a team led by Piero Anversa, MD, at the Brigham and Women's Hospital in Boston to perfect a technique for using a patient's own cardiac stem cells to regenerate dead heart muscle after a heart attack.
In honor of his illuminating work, the American Physiological Society (APS) has selected Dr. Bolli to present the Walter B. Cannon Memorial Lecture at the Experimental Biology 2011 meeting (EB 2011). This lecture is the Society's pre-eminent award lecture and is designed to recognize an outstanding scientist for his or her contributions to the field.
A Tale of Two Proteins
The cardiac stem cell treatment investigated in the SCIPIO trial consists of isolating the patient's cardiac stem cells from part of the upper chamber of the heart (harvested during coronary bypass surgery) and expanding these cells in the lab. Four months after surgery, the cells are infused into scarred cardiac tissue by catheterizing a large artery in the patient's leg. Using the patient's own cardiac stem cells eliminates the possibility of rejection.
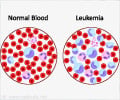
Besides SCIPIO, Dr. Bolli is also performing basic research aimed at on enhancing the cardiac stem cells while they are cultured in the lab for expansion. He is working with two proteins, heme oxygenase 1 (HO-1) and nitric oxide synthase (NOS). HO-1 is a protein made in response to cellular stress, such as oxidative stress or oxygen deficiency. It catalyzes the breakdown of heme, which is a molecular component of hemoglobin, the part of the red blood cell that transports oxygen around the body. When HO-1 breaks down heme, one of the by-products is carbon monoxide (CO). NOS, the other protein Dr. Bolli is investigating, is an enzyme that catalyzes the production of nitric oxide (NO). Dr. Bolli is focusing on these two proteins because their catalytic by-products, CO and NO, exert remarkable beneficial effects.
Advertisement
A Promising Future
Advertisement
Even with natural cells (in which these proteins are not increased), such as those used in SCIPIO, the results are very encouraging. Improvements seen in patients who have received cardiac stem cell infusion include increased ejection fraction, the fraction of blood pumped through the two lower chambers of the heart. Patients also experience dramatic improvements in what they are able do physically, Dr. Bolli says. "There are people who are almost completely incapacitated, and after they get stem cells, they can do so much more. I have a patient who couldn't walk to the bathroom, and now he can walk two miles."
Dr. Bolli cautions that SCIPIO is a Phase 1 trial, meaning that it is the first round of testing in humans. Its primary purpose is to assess safety and feasibility, rather than efficacy. Yet, he remains optimistic and notes that cardiac stem cells offer the hope of healing the heart. "All of the other treatments currently available--transplants, assist devices, drugs--may prolong life but do not solve the problem. By regenerating new heart muscle, cardiac stem cells could actually solve the problem."
To date, 17 patients have received cardiac stem cells in the SCIPIO trial. Dr. Bolli will discuss his research and provide the latest details of how the patients are faring when he presents this year's Cannon Lecture, "The nitric oxide–carbon monoxide module: A fundamental mechanism of cellular resistance to stress," on Saturday, April 9, 5:45 pm ET at the Walter E. Washington Convention Center.
Walter B. Cannon Award Lecture
The Cannon Award lectureship, established in 1982, is the APS' highest award. The individual selected is an outstanding physio¬logical scientist chosen by the President-Elect, with the consent of Council, to lecture on "Physiology in Perspective" during the plenary session of the Society's next annual meeting. At the 1984 fall meeting, the title of the presentation was changed to "Physiology in Perspective: The Walter B. Cannon Lecture."
Source-Eurekalert