‘Direct oral anticoagulant (DOAC) drugs used for blood clots have shown improved efficacy and a decreased risk of major bleeding.’
Tweet it Now
Cancer can increase the risk of blood clots and treatments such as chemotherapy can further increase the risk. Cancer patients with CAT face double the mortality rate compared to cancer patients without thrombosis. It also adds a significant financial burden for these patients.For many years, injection of low molecular weight heparin has been the treatment of choice in patients who have cancer-associated thrombosis. The DOACs came on scene eight or nine years ago and are considered to have better safety and efficacy profiles.
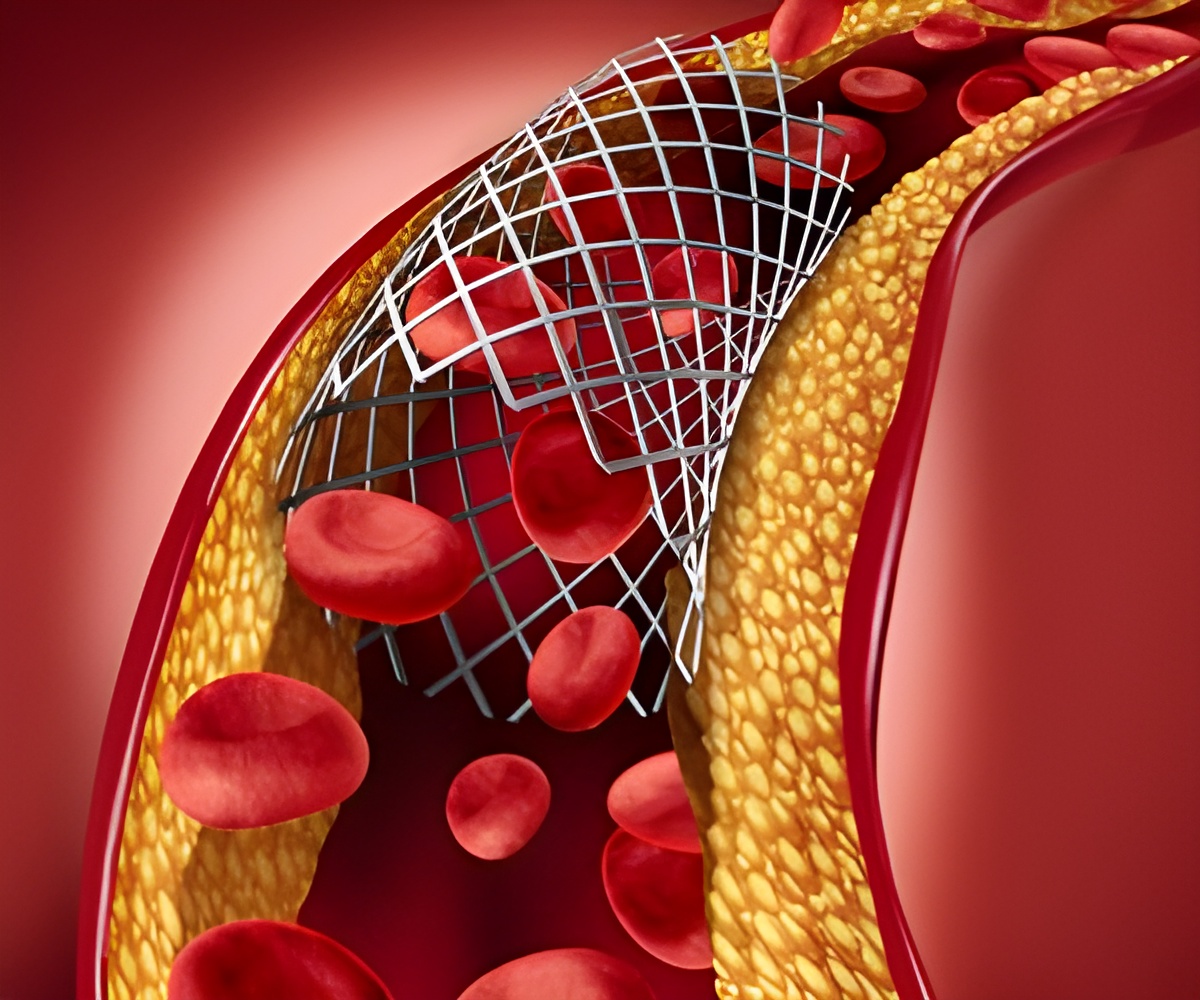
Clinical trials have shown improved efficacy and a decreased risk of major bleeding with the DOACs, but the question is whether people will be willing to pay the additional cost to get a better outcome.
These drugs were compared head-to-head using a computer model that simulates major health events that happen to a cohort of patients with cancer over time who have experienced a blood clot.
Then, throughout the lifetime of the patient cohort, the study examined the accumulating lifetime costs and lifetime effectiveness measured in a metric called quality-adjusted life years (QALYs).
Oral Anticoagulants are Better than Low Molecular Weight Heparin
In the base-case analysis, using the cost of drugs purchased at a federal facility such as the Veteran’s Administration, apixaban was favored as being more effective and less costly than either LMWH or edoxaban while indicating rivaroxaban was not cost-effective.Advertisement
In this scenario, if decision-makers were unwilling to spend more than $50,000 per QALY, edoxaban was favored and using the contemporary threshold for societal willingness to pay, rivaroxaban was cost-effective, with an incremental cost-effectiveness ratio of just more than $50,000 per QALY.
Advertisement
An individual’s insurance coverage plan can make a huge difference in the patient’s out-of-pocket costs for these medications.
Source-Eurekalert