‘Anti-stroke drug 3K3A-APC reduces the incidence of hemorrhage in patients with acute ischemic stroke.’
Tweet it Now
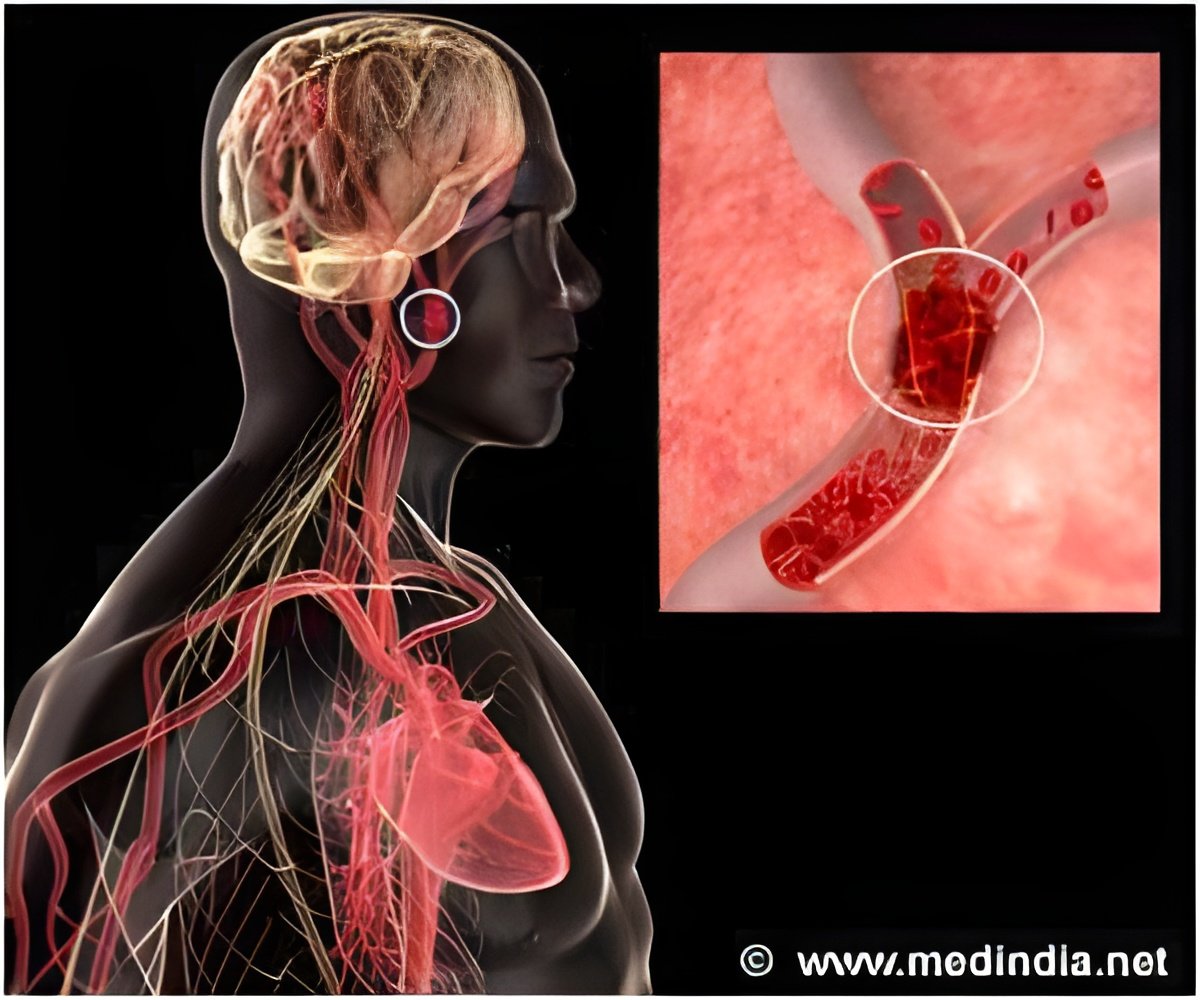
Stroke is the fifth leading cause of death in the United States and the number one cause of adult disability. Acute ischemic strokes occur when a clot blocks blood flow to the brain. To date, the FDA has approved only one drug treatment, called tissue plasminogen activator (tPA), to treat acute ischemic strokes. tPA helps break up blood clots if given within a 4.5-hour window after the stroke. Unfortunately, tPA's use is limited due to this brief treatment window and its potential to cause bleeding in the brain and neuronal cell death. But studies so far show that 3K3A-APC could complement tPA administration. Griffin designed the experimental drug by modifying just three amino acids on a naturally occurring blood protein called protein C, which is both an anticoagulant and a cell protective agent.
"This is an extremely novel drug," says Griffin.
Preclinical testing in collaborative studies involving Griffin's lab and the lab of Berislav Zlokovic, MD, PhD, director of the Zilkha Neurogenetic Institute at the University of Southern California, showed that 3K3A-APC lessens the damage of stroke and protects brain cells from the side effects of tPA. The drug was licensed by TSRI to the pharmaceutical company ZZ Biotech, where Zlokovic was the scientific founder.
To find the maximally tolerated dose, the National Institutes of Health's National Institute of Neurological Disorders and Stroke (NINDS) funded the recent Phase 2 study, called RHAPSODY, through a grant to the principal investigator Patrick Lyden, MD, chair of the Department of Neurology at Cedars-Sinai in Los Angeles, and through a NeuroNEXT Infrastructure Resource Access grant to ZZ Biotech, where Kent Pryor, PhD, served as co-principal investigator. NINDS entered into a Cooperative Research and Development Agreement (CRADA) with ZZ Biotech.
Advertisement
As a secondary endpoint, the researchers evaluated cerebral hemorrhage in these patients. They found that total hemorrhage volume and hemorrhage incidence were both substantially reduced in 3K3A-APC-treated patients. The incidence of any hemorrhage was reduced from 86.5 percent in placebo-treated patients to 67.4 percent in the combined treatment arms. Total hemorrhage volume was likewise reduced from an average of 2.1±5.8 mL on placebo to 0.8±2.1 mL in the combined treatment arms.
Advertisement
Griffin says the collaborative environment at TSRI made the development of 3K3A-APC possible. "I've been blessed by working with fantastic people. TSRI has been committed to basic research and discovery of new knowledge, especially with translational potential--and that's been my philosophy."
Source-Eurekalert