But Gladstone postdoctoral scholar Li Qian, PhD, along with researchers in the laboratory of Deepak Srivastava, MD, has now accomplished this transformation in living animals-and with even greater success.
The results may have broad human-health implications.
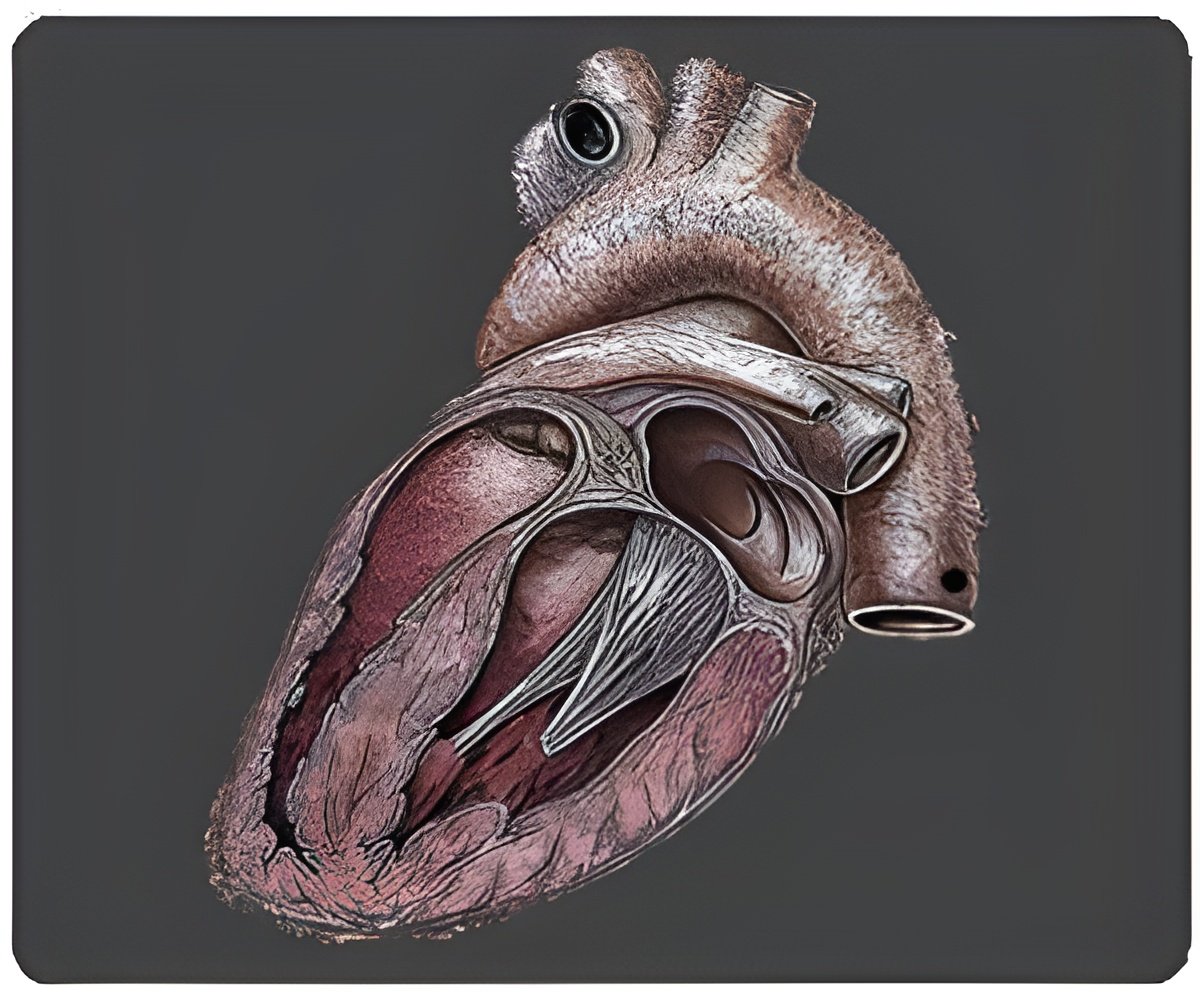
"The damage from a heart attack is typically permanent because heart-muscle cells-deprived of oxygen during the attack-die and scar tissue forms," said Dr. Srivastava, who directs cardiovascular and stem cell research at Gladstone, an independent and nonprofit biomedical-research institution.
"But our experiments in mice are a proof of concept that we can reprogram non-beating cells directly into fully functional, beating heart cells-offering an innovative and less invasive way to restore heart function after a heart attack."
In laboratory experiments with mice that had experienced a heart attack, Drs. Qian and Srivastava delivered three genes that normally guide embryonic heart development-together known as GMT-directly into the damaged region.
Advertisement
"These findings could have a significant impact on heart-failure patients-whose damaged hearts make it difficult for them to engage in normal activities like walking up a flight of stairs," said Dr. Qian, who is also a California Institute for Regenerative Medicine postdoctoral scholar and a Roddenberry Fellow.
Advertisement
"Our next goal is to replicate these experiments and test their safety in larger mammals, such as pigs, before considering clinical trials in humans," said Dr. Srivastava, who is also a professor at the University of California, San Francisco (UCSF), with which Gladstone is affiliated.
"We hope that our research will lay the foundation for initiating cardiac repair soon after a heart attack-perhaps even when the patient arrives in the emergency room," Dr. Srivastava added.
The study has been published in the journal Nature.
Source-ANI