‘Developing new and innovative drugs that target miRNA181a and NFAT5 can limit islet autoimmunity.’
Tweet it Now
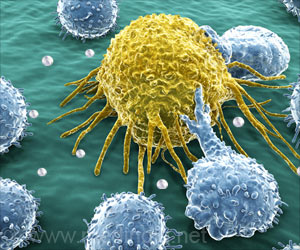
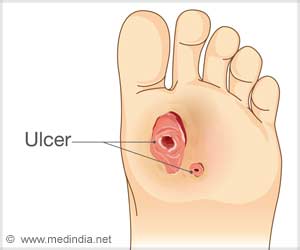
Regulatory T cells (Tregs) play an important role in this process: In healthy people, they suppress excessive immune reactions and thus prevent autoimmune diseases.Dr. Carolin Daniel's team is investigating why Tregs fail to protect the islet cells in type 1 diabetes. She is a group leader at the Institute for Diabetes Research (IDF) of Helmholtz Zentrum München and a scientist in the DZD.
In the current study, she and her team elucidated a mechanism that causes fewer Tregs to be produced during islet autoimmunity onset and that therefore allows the immune system to get out of control and attack.
According to the findings of the study, miRNA181a and NFAT5 molecules play a key role. "We showed that miRNA181a leads to the activation of the transcription factor NFAT5 during islet autoimmunity onset," said Daniel. "The consequence is an inhibition of Treg induction and thus increased immune activation."
Axis pharmacologically interrupted
Advertisement
If the researchers interrupted the miRNA181a/NFAT5-axis, they observed a significantly lower activation of the immune system and an increased formation of Tregs. This was achieved both by the pharmacological inhibition of miRNA181a as well as of NFAT5.
Advertisement
"The combination with other immune modulating therapeutic approaches would also be conceivable as an intervention."
In the future, the scientists want to further investigate these findings in preclinical tests.
To this end, humanized models will be used to test whether the combination of insulin vaccination and inhibition of the miRNA181a/NFAT5 axis leads to a more tolerant immune system towards insulin-producing cells.
Source-Eurekalert