Administration of antiretroviral drugs with an antibody during and after drug treatment can help achieve sustained control of infection by SIV in rhesus macaques.
‘Administration of the antibody alpha4-beta7 integrin can block SIV (simian immunodeficiency virus) transmission in a significant number of rhesus macaques.’





Members of the research team at Department of Pathology, Emory University School of Medicine and the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, report that the virus is still present in the bodies of the antibody-treated monkeys. Yet it has stayed below the limit of detectability in their blood, lasting almost two years after withdrawal of antiretroviral drugs.The antibody, the team, used was designed to stop susceptible immune cells from entering intestinal tissues, a hot spot of damage during acute HIV and SIV infection. An analogous human antibody called vedolizumab was FDA-approved for the treatment of Crohn's disease and ulcerative colitis in 2014. Based on the current findings, a pilot clinical trial, testing the safety of vedolizumab and its effect on HIV in people infected with the virus, has begun at NIAID.
"This comes from an idea I had many years ago: stopping CD4+ T cells from circulating into the gut may protect them during acute infection," says senior author Aftab Ansari, PhD, professor of pathology and laboratory medicine at Emory University School of Medicine and Yerkes National Primate Research Center. "But how it works in the setting of chronic infection is still far from clear. The antibody appears to have helped the entire immune system rebuild itself."
The co-first authors of the paper are Emory researcher Siddappa Byrareddy, PhD, now an associate professor at University of Nebraska Medical Center, and James Arthos, PhD, and Claudia Cicala, PhD both of the Laboratory of Immunoregulation. Arthos and Cicala worked under the overall direction of co-author Anthony Fauci, MD, director of NIAID. The study was conducted at Yerkes National Primate Research Center, Emory University. Collaborators at University of Maryland, University of Michigan and the German Primate Center contributed to the paper.
Several questions remain. How long can remission last? Which parts of the immune system are most important for viral control? And what differences between this experiment and HIV infection of humans might impede translation of this finding into the clinic?
Advertisement
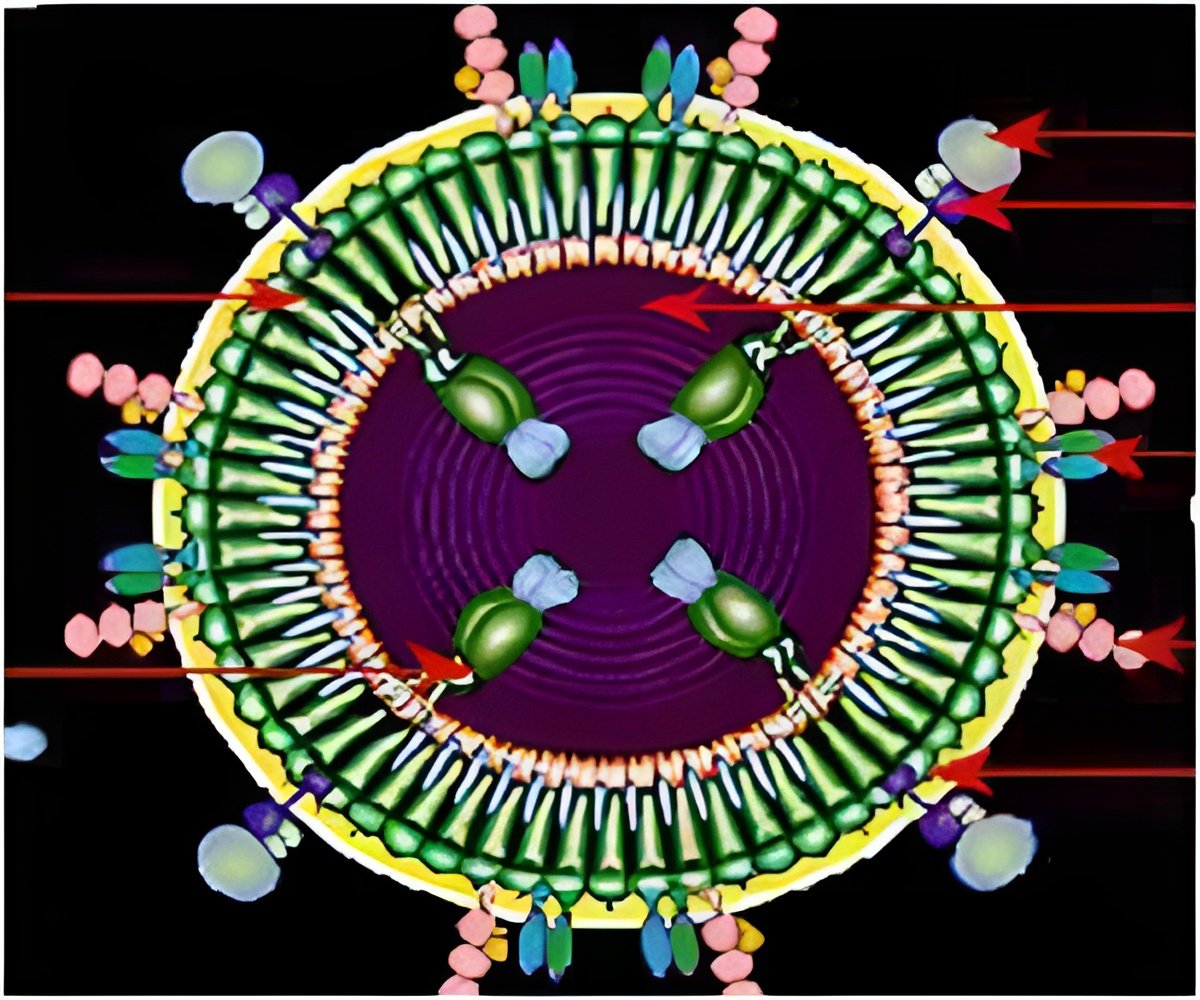
In the Science paper, the antibody the team used is against alpha4-beta7 integrin, which helps T cells find their way to intestinal lymphoid tissues. In 2008, NIAID researchers identified alpha4-beta7 integrin as a cell surface molecule involved in the association of the virus envelope with CD4+ T cells, but the antibody does not appear to directly block viral entry. Previous research has shown that the administration of the same antibody can block SIV transmission in a significant number of rhesus macaques.
Advertisement
At week 9, four weeks after starting on antiretroviral drugs, 18 monkeys began to receive infusions of the alpha4-beta7 antibody or control antibodies, every three weeks. Three developed antibodies against the alpha4-beta7 antibody and were excluded from further study. Drugs were withdrawn at week 18 and antibodies at week 32. When antiretroviral drugs were stopped, SIV came roaring back in the seven control animals. Six of eight alpha4-beta7 treated animals also showed some rebound of viral levels, but they controlled it within four weeks. The other two never even rebounded.
In the alpha4-beta7-treated monkeys, the researchers observed a gradual restoration of CD4+ T cells, the main target cells for the virus, and other immune cells. The team used a PET/CT imaging technique, developed by co-authors Philip Santangelo, PhD at Georgia Tech and Francois Villinger DVM, PhD at Yerkes, to visualize CD4+ T cells throughout the body.
Also, in the alpha4-beta7-treated monkeys, the team did not see neutralizing antibodies. HIV vaccine designers have made a goal of stimulating neutralizing antibodies, which may be able to prevent a nascent viral infection.
However, the researchers did see non-neutralizing antibodies against part of the envelope protein of SIV called the V2 loop. Antibodies against the V2 loop of HIV were beneficial in the RV144 study in Thailand, the only HIV vaccine study to demonstrate partial protection against infection.
"This finding could become a blueprint for an alternative therapy for HIV, which could make it so someone would not need to continuously take anti-retroviral drugs," Ansari says. "It could also help us craft more effective vaccines. We need to know more about how alpha4-beta7 antibody treatment exerts its effects."
Additional experiments are planned to determine which parts of the alpha4-beta7-treated macaques' immune systems are critical for maintaining control of SIV, he adds.
Before withdrawal of antiretroviral drugs, the alpha4-beta7-treated animals showed a restoration of the levels of retinoic acid, a derivative of vitamin A, and other immune regulators. Potentially, biomarkers like these could help predict whether someone's immune system is ready for stopping anti-retrovirals.
The results are published in Science.
Source-Eurekalert