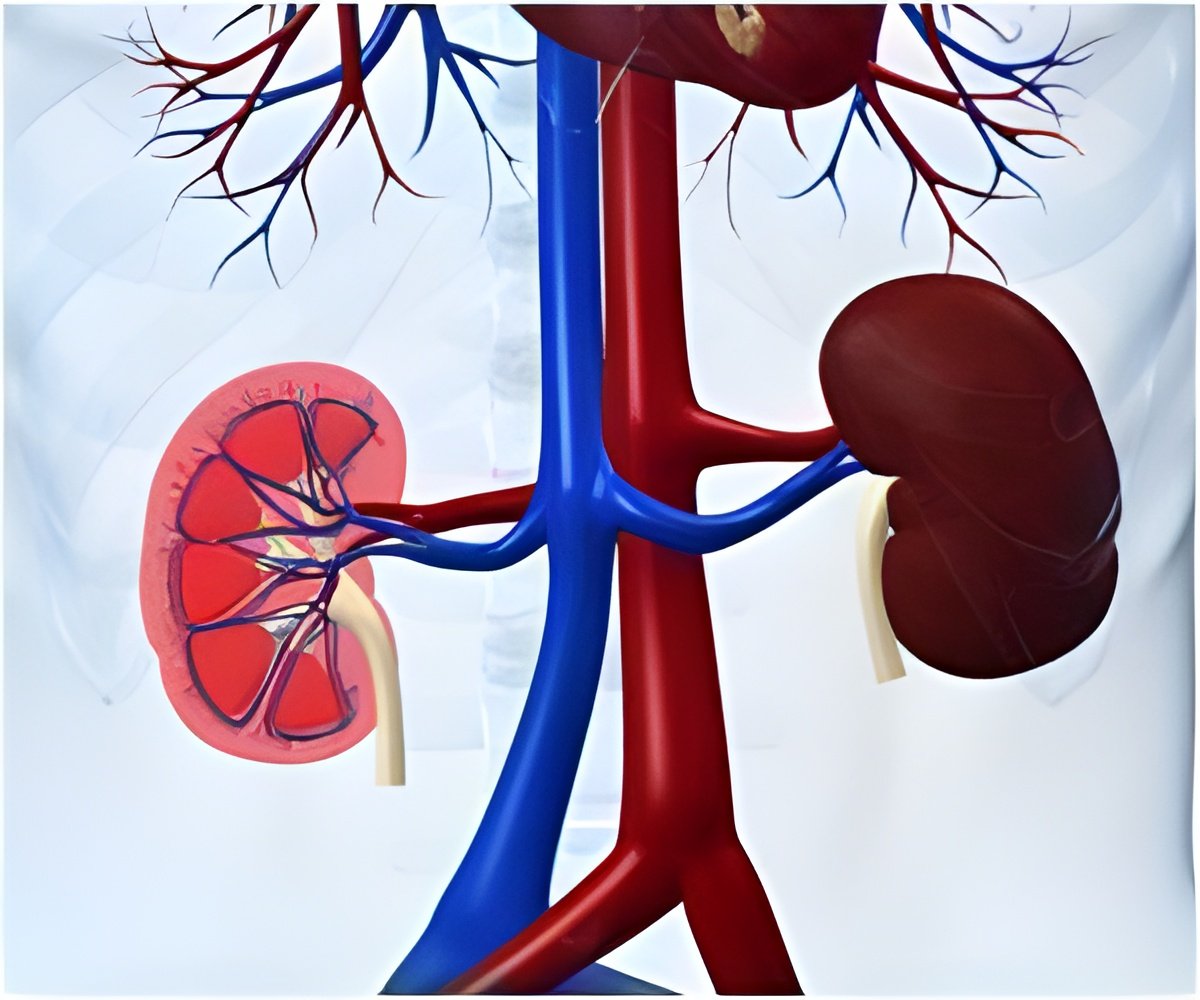
For patients whose kidneys no longer work, hemodialysis performs the work of the kidneys. Experts recommend creating an arteriovenous fistula (AVF), to connect a vein and artery and allow access to the vascular system. An AVF provides a long-lasting site through which blood can be removed and returned during the dialysis procedure, which patients must undergo 3-4 times per week.
While AVF use for hemodialysis access is safe, cost-effective, and associated with improved survival in kidney disease patients, only a minority of US patients start hemodialysis with an AVF (13.7% in 2008).
Frank Hurst, MD (Walter Reed Army Medical Center and F. Edward Hebert School of Medicine) and his colleagues evaluated the use of AVFs in federally sponsored national health care organizations such as the Departments of Veterans Affairs (DVA) and Department of Defense (DoD). Dr. Hurst and his team searched the United States Renal Data System (USRDS) database to identify patients who initiated hemodialysis between 2005 and 2006. They found that patients who received predialysis kidney care were 10 times as likely to begin dialysis with an AVF compared with patients who did not receive such care. Patients with DVA/DoD insurance were 40% more likely to initiate dialysis with an AVF compared with patients with other types of insurance. Specifically, 27.2% of patients with DVA/DoD insurance initiated hemodialysis with an AVF, compared with 18.5% of patients reporting employer-group insurance, 16.7% of patients with "Other" insurance, 15.6% of patients with Medicare, 13.0% of patients with Medicaid, and 8.2% of patients who reported no insurance. The analysis also revealed that patients who initiated hemodialysis at a DoD facility were twice as likely to use an AVF.
Experts are attempting to increase the use of AVFs through initiatives such as the Fistula First Breakthrough Coalition, whereby the Centers for Medicare & Medicaid Services, End Stage Renal Disease Networks, and the entire kidney community are working together to ensure that every suitable patient will receive the most optimal form of vascular access. Dr. Hurst's findings show that despite these efforts, AVF use is still highly dependent upon a patient's type of health insurance prior to the initiation of dialysis.
"Further study of these federal systems may identify practices that could improve processes of care across healthcare systems to increase the number of patients who initiate hemodialysis with an AVF," the authors wrote. They added that while AVF use is more frequent in DVA/DoD patients, the proportion of these patients who initiate hemodialysis with an AVF is still far too low.
Advertisement
In an accompanying editorial, Steve Schwab, MD and Kennard Brown, PhD (University of Tennessee Health Science Center) expressed dismay that AVF placement before dialysis, which requires treatment by both a nephrologist and a vascular surgeon, is not covered by Medicare, which supports most coverage for dialysis. "We now have a public policy that treats a catastrophic illness such as renal failure but does not act to prevent or ameliorate that catastrophe earlier," they wrote. The authors advocate for amending policy guidelines so that patients can benefit from seeing specialists early in the course of their disease.
Advertisement
Source-Eurekalert