- Dysmenorrhea - (http://emedicine.medscape.com/article/253812-overview#a0101.)
About
Pain during menstrual periods may be due to a uterine or pelvic cause, especially in older women.
Pain that accompanies cyclic menstrual periods is called dysmenorrhea. It interferes with routine life especially in young girls. Ten percent women are actually incapacitated for 1 to 3 days each month due to painful menstruation. Menstrual pain may also be present in older women; these cases are often due to a specific cause. Older women should therefore undergo testing to find out the cause of the pain, especially in the case of new onset pain.

The causes of primary and secondary dysmenorrhea are listed below:
Primary Dysmenorrhea:
Primary dysmenorrhea usually affects young girls. It occurs due to the release of hormone-like substances called prostaglandins during menstruation. The prostaglandins result in contraction of the uterine muscles. The blood vessels thus get compressed leading to reduced blood supply to the muscles. This results in pain.
Prostaglandins are released during cycles in which the ovum or egg is released. In the first year of menstruation, the egg may not be released in all the cycles, i.e. the cycles may be anovulatory. These cycles are usually painless.
The pain in primary dysmenorrhea is usually most severe on the first day and may feel like severe cramps. It usually lasts for 1 to 2 days. It may be accompanied by nausea, vomiting, loose stools, dizziness, headache and fatigue.
Secondary Dysmenorrhea:
Secondary dysmenorrhea usually occurs due to a problem in the female reproductive organs or the pelvis. It is usually seen in older women. The symptoms usually begin just before the bleeding starts and last till just after the bleeding has stopped. Causes of secondary dysmenorrhea are listed below:
- Conditions that affect the pelvis:
- Endometriosis: Endometriosis is a condition where the cells similar to those lining the uterus grow outside the uterus. They also undergo changes under hormonal influence, like the uterine lining, and bleed during the menstrual cycle, giving rise to pain.
- Pelvic inflammatory disease: Pelvic inflammatory disease refers to infection of the uterus, fallopian tubes, ovaries or the pelvis. The infection may travel up from the vagina and cervix, as in the case of sexually transmitted diseases, or may follow childbirth or surgical procedures. Along with menstrual pain, pelvic pain, fever and vaginal discharge may be present.
- Pelvic congestion syndrome: Pelvic congestion syndrome occurs due to the presence of dilated veins in the pelvis. The pain is felt during menstrual periods, following intercourse, prolonged standing or during pregnancy. Associated symptoms may include abnormal menstrual bleeding, irritable bladder, vaginal discharge and dilated veins in the vulva, buttocks and thighs.
- Allen-Masters syndrome: Allen-Masters syndrome is condition where the pelvic muscles are damaged and allow excessive motility of the cervix. The damage is often a result of traumatic deliveries.
- Conditions that affect the uterus
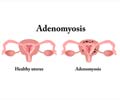
- Adenomyosis: Adenomyosis is a condition where the lining of the uterus grows into the muscle wall. Along with severe menstrual pain that lasts throughout the period, the patient may also experience heavy bleeding with bleeding between periods and pain during intercourse.
- Fibroids: Fibroids are benign muscle tumors arising from the uterine wall. Along with menstrual pain, they also cause excessive bleeding, pelvic discomfort and pain, pain during intercourse and symptoms due to pressure over the bladder and rectum.
- Uterine polyps: Uterine polyps are small growths that arise from the uterus and remain attached to the uterus by a thin stalk. They may cause excessive and irregular menstrual bleeding and may be one of the causes of infertility.
- Intrauterine adhesions: Damage to the inner lining of the uterus results in the formation of scar tissues and adhesion between the walls of the uterus. The damage occurs usually due to surgical procedures like dilatation and curettage (D&C) or removal of fibroids. It could also occur due to insertion of an intrauterine device like Copper –T or infection of the uterus. The patient suffers from infertility or repeated miscarriages. Pain may occur during menstruation if the adhesions cause obstruction to the flow of menstrual blood.
- Congenital malformations: The presence of congenital abnormalities in the uterus like bicornate uterus (uterus with two horns) and subseptate uterus (uterus with a partition within) can result in painful menstruation.
- Intrauterine contraceptive device: An intrauterine contraceptive device like Copper-T could cause cramps during menstruation.
- Conditions that affect the cervix and vagina
- Cervical stenosis or occlusion: Cervical stenosis is a condition where the opening of the uterine cervix is narrowed, either partially or completely. It may be a condition present from birth or may arise later in life due to trauma, surgical procedures, infections, cancer or radiation. The patient is at an increased risk for infertility and endometriosis.
- Transverse vaginal septum: A transverse vaginal septum occurs as a birth defect. The menstrual blood is unable to flow out due to the septum leading to menstrual cramps.
- Conditions that affect the ovaries
- Ovarian cysts and tumors: Ovarian cysts are fluid-filled sacs in the ovary which are usually benign but may rarely be cancerous. They may, in addition, cause symptoms like irregular menstruation, discomfort during intercourse and problems with bowel and bladder function.
FAQs
1. Which doctor should I visit in case I have painful menstrual periods?
You should visit a gynecologist to get treated for painful menstrual periods.
2. How are painful menstrual periods treated?
If there is a definite cause for the painful menstrual periods, then treating the cause can provide relief. Over-the-counter painkillers may be used to treat primary dysmenorrhea. Hormonal treatment with oral contraceptives may help in cases not responding to painkillers. General measures like application of heat, self massage over the lower abdomen, a healthy diet, regular exercise and stress reduction may also be helpful.
3. Are there any risk factors associated with painful menstruation?
Some factors that could be associated with more severe pain during menstruation are an early age at menarche, long menstrual periods, heavy menstrual flow, having no children in the past, a positive history of painful menstruation of other women in the family, obesity, smoking and alcohol consumption.