What is Cervical Ripening?
Normal labor is the process of expulsion of a viable fetus to the outside world. This process begins with the commencement of true labor contraction and ends with the expulsion of the placenta.
Normal labor is the process of expulsion of a viable fetus to the outside world. This process begins with the commencement of true labor contraction and ends with the expulsion of the placenta.
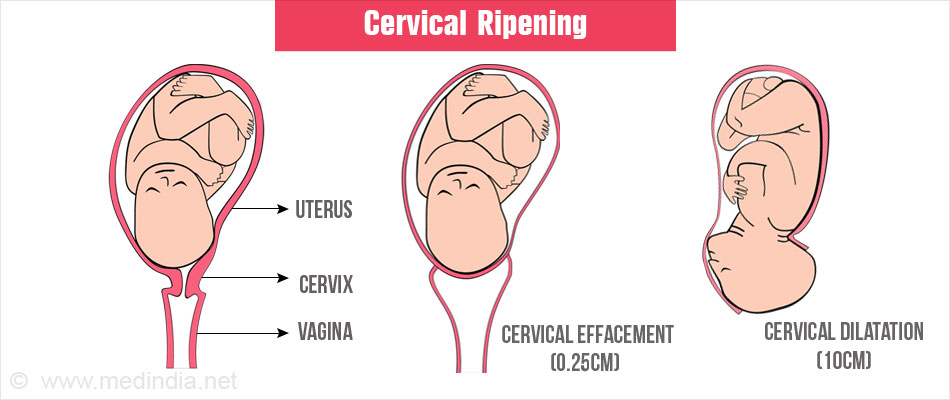
An important event which takes place during the initial stages of labor is called cervical ripening. It consists of softening, dilatation and shortening of the cervical canal in order to push the baby out without any obstruction. These steps have to happen in synchrony with the uterine contraction and decent of the baby’s head. When this process is delayed or not in synchrony or there is an emergent need to terminate the pregnancy, induction and cervical ripening have to be done artificially so as to have a healthy labor.
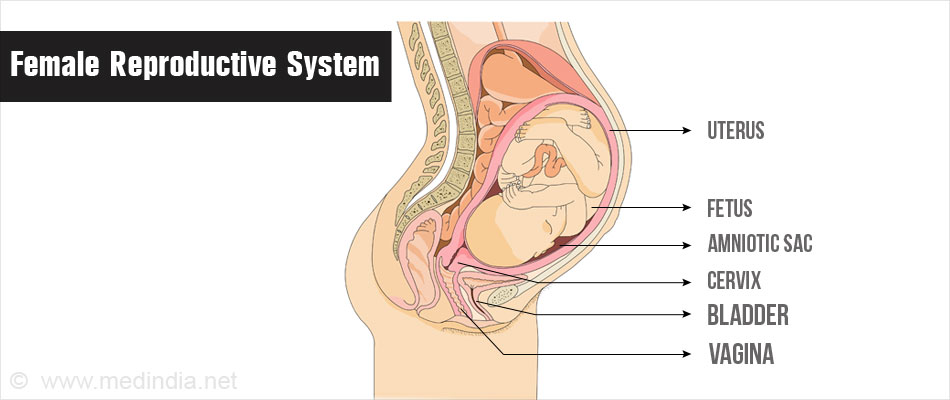
Female Reproductive Tract
The female reproductive system primarily consists of 2 ovaries on either side of the pelvis which open into a dome shaped cavity called uterus. This uterine cavity is where the baby grows during pregnancy. The outer opening of the reproductive tract is the vagina. The cervix is a cylindrical passage which connects the uterus to the vagina.
It is a tubular organ made of fibrous connective tissue in continuation with the myometrium and endometrium of the uterus, which measures to around 2.5-3cm in length. The inner surface, called the endocervix, is lined by a layer of mucus secreted by the glandular cells of the cervix. Another important feature of the cervix is that it is insensitive to heat and touch.
Changes in the Cervix During Pregnancy
Physiological changes occur in the cervix during pregnancy which helps in holding the fetus inside the uterus and also help pushing the baby out during the process of labor. During pregnancy there is an increase in the size and mass of the muscular tissue and glandular cells of the cervix. Due to this hyperplasia of the glands the mucus secretion in the cervix increases and becomes tenacious. To accommodate these changes the blood flow to the cervix also increases. The above mentioned changes are clinically visible from 6 weeks of pregnancy. Though the width of the cervix increases the length remains the same and the cervical opening remains closed until towards the end of the pregnancy.
Changes in the Cervix During Child Birth
Towards the end of the pregnancy period, just before the onset of labor, the cervix starts becoming soft and the length starts reducing. The cervical canal becomes dilatable and usually admits one finger which keeps dilating further during labor to let the rigid head pass through. When the baby starts coming out, the cervix becomes fully effaced and reduced to less the 1.5cm.
Dilatation of the Cervix
Prior to onset of labor there may be certain amount of dilation of the cervix in multigravida (woman who has been pregnant more than once) and in some primigravida (woman pregnant for the first time). But in general, cervix dilation starts at the first stage of labor, along with or after the commencement of true labor contractions. This is accompanied by a process called effacement during which the cervix gets pulled up and merges with the lower uterine segment. These two processes help in letting the baby pass through the narrow passage. Cervix softening along with effacement and dilation is called cervical ripening. The final phase of the dilatation is carried out by the downward thrust of the expelling fetus. With complete dilatation the second stage of labor starts and expulsion of baby begins.
Factors Responsible for Physiological Cervical Ripening:
Cervical ripening is measured in terms of cervical dilatation, cervix length, consistency of the cervix and position of the cervix in relation to the uterus. These measures along with the rate of descent of the head are together known as Bishop scoring. This scoring method tells us the status of the cervix, whether the baby’s head will be able to pass through and whether induction is needed.
Effacement: The process of effacement refers to the shortening of length of the cervix. It starts after the rupture of the amniotic membranes. Effacement of the cervix is expressed in terms of percentage, i.e. 25%, 50% or 100% (cervix less than 0.25 cm length).
Dilatation: Cervical dilatation is expressed in terms of how many fingers the cervix allows i.e., 1,2 and 3 fingers. Each finger corresponds to an average of about 1.6cm. More than 3 fingers refers to the cervix being fully dilated (around 10cm).
Labor induction refers to the initiation of uterine contraction and cervical ripening by any method, beyond the period of viability, for the purpose of vaginal delivery. Induction maybe used synonymously with ripening. Indication for an induction is when the continuation of pregnancy is harmful to either the fetus or the mother or both.
Indications:
A) Pharmacological:
These are cervical softening medications which inturn help in dilation and effacement. These medicines may be given orally, intravenously or per vaginam (through the vagina).
They are:
Prostaglandins have great importance in obstetric practice because of the ability to induce uterine contraction and also aid in cervical ripening. They can be administered orally as well as vaginally although vaginal administration is much more effective than oral. Most common prostaglandins used are PGE1(misoprostol), PGE2 (dinoprostone) and PGF2á. PGE1 and PGE2 are primarily used as cervical ripening agents whereas PGF2á is used to induce uterine contraction.
Dosage: Misoprostol (also called cytotec induction) is usually given as 25mcg vaginally every 4hrs upto 6-8 doses.
Dinoprostone is a gold standard for cervical ripening and is given as 0.5mg vaginally every 6hrs for upto 3-4 doses. The mother should be on complete bed rest after its administration and uterine contraction is monitored.
Side effects of these drugs include hyperstimulation of the uterus, passage of stools by the fetus and might also lead to uterine rupture. Hence it is contraindicated in mothers with history of previous cesarean section.
B) Surgical or Mechanical Methods:
This is done either by rupturing the amniotic membrane, separating the membranes or by using a mechanical dilators.
C) Non-pharmacological Methods:
These are traditional non-medical methods that can be followed even at home.
Risks and Benefits of Induction
Risks to the mother:
Risks to the baby:
Benefits:
Potential benefits include:
Simple health tips to promote natural vaginal delivery without the need for induction or cesarean section include: