Treatment and Follow-up for Thyroid Cancer
Treatment
An early diagnosis allows better cure of most thyroid cancers. A number of options are available, and are literally ‘customised’ to the needs of the individual.
The following factors are taken into account:
- The type of cancer
- The size of the nodule
- Age of the patient
- The spread of the cancer
In this context it would be wise to just know that there is the so called AGES or AMES criteria to categorise a patient as belonging to a high risk or a low risk group. This considers factors like:
- Age
- Sex
- Size
- Spread of the tumour
- Grade of the tumour
A tumour may be well differentiated or poorly differentiated. You needn’t ponder deep into these aspects.
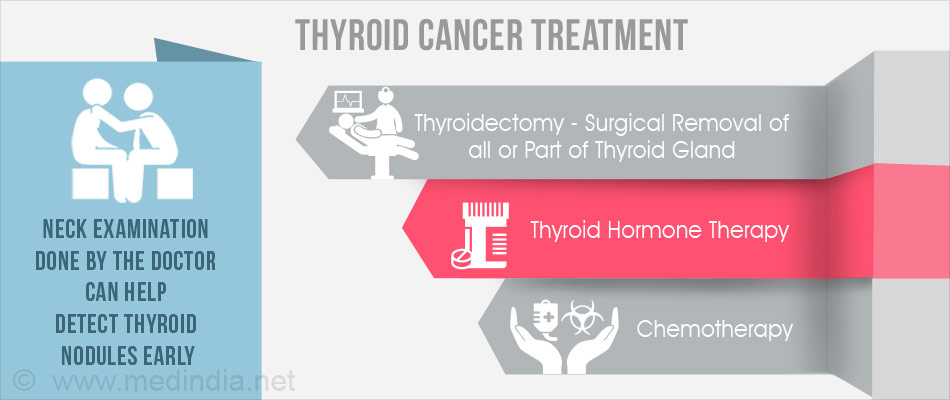
Available treatment modalities include:
- Surgery
- Thyroid hormone treatment
- Radioactive iodine therapy
- External radiation therapy
- Chemotherapy
Patients usually require a combination of the above mentioned options. The decision is made based on various factors. For example a papillary cancer may require a combination of surgery, hormone treatment and radioactive iodine therapy.
Surgery and External radiation therapy are ‘local’ modalities that destroy the cancer in the thyroid or in the local regions to which it has spread.
The others (thyroid hormone treatment, radioactive iodine therapy and chemotherapy) are ‘systemic’ therapies which traverse the whole body and destroy (or control) the cancer throughout.
You should also know that the treatment modalities are not immune to the development of side effects.
Surgery - Thyroidectomy:
This is the commonest modality. The surgeon may remove whole or part of the gland. When the whole gland is taken it is called Total Thyroidectomy. This may be done in all types of thyroid cancers. Depending upon the status of the patient it may be followed by removal of lymph nodes, radioactive iodine therapy, external radiation therapy etc.
Variants of Total Thyroidectomy are Near-total Thyroidectomy, sub-total Thyroidectomy. The surgery is named based on the amount of tissue removed. Terminology of thyroid surgery is inconsistent in literature.
Sometimes only one lobe needs excision. This is lobectomy (the isthmus is also removed). Thus the type of surgery is dependent on the patient’s disease status.
Following surgery the patient may require thyroid hormone replacement therapies, second surgeries, or further radiation. Note that I have stressed the ‘MAY’ part!
The surgery may involve complications like accidental removal of parathyroid glands(remember the location, mentioned in the first page) in which case calcium and vitamin D supplements may be indicated. Voice changes or hoarseness may be the results of damage to important nerves. But these complications rarely happen in the hands of competent surgeons.
Thyroid Hormone Replacement:
Most people require hormone replacement following thyroid surgeries. Thyroid hormone pills slower the growth of cancer cells left behind after surgeries. The dosage need to be adjusted by the doctors, and NOT by the patient since too less or too high doses may do harm. Otherwise, side effects are rare.
Radioactive Iodine Therapy (I-131):
This is of value to patients with papillary or follicular thyroid cancer. It kills the thyroid cancer cells and normal tissue left after surgeries. Medullary or Anaplastic cancers do not respond to this treatment.
Points worth noting about the Radioactive Iodine Therapy (I-131) are:
- Even people who are allergic to iodine may safely take up this therapy
- Given in the form of a liquid or a capsule that is swallowed
- Stay at the hospital may not be mandatory
- The health team is to be consulted to learn how to protect the family members and co-workers from exposure to radiation.
- Drinking lots of fluids during the therapy. This protects the bladder.
- Some people have mild nausea the first day of I-131 therapy.
- A few people have swelling and pain in the neck where thyroid cells remain. If thyroid cancer cells have spread outside the neck, those areas may be painful too.
- A dry mouth or lose of sense of taste or smell for a short time after I-131 therapy may occur. Chewing sugar-free gum may help in this situation.
- Loss of fertility is a rare side effect in men who receive a high dose of I-131.
- Though I-131 may not cause loss of fertility in women some doctors advise to avoid getting pregnant for one year after a high dose of I-131.
- It has been reported that a very small number of patients may develop a second cancer years after treatment with a high dose of I-131.
- After radioactive iodine therapy, the patient may need to take thyroid hormone pills to replace the natural hormone.
External radiation therapy (or radiotherapy):
This is done when surgery or I-131 therapy can’t be used, or when they fail. Here cancer cells are killed using high energy radiations. The side-effects of this treatment may be distressing but are controllable. Most side-effects disappear after the end of treatment.
Chemotherapy:
This is often required in anaplastic cancers. Chemotherapy may also be used to relieve symptoms in other thyroid cancers. Side-effects vary depending upon the drugs used. The most common ones being nausea, vomiting, mouth sores, loss of appetite, and hair loss. These are controllable and may not persist once the treatment is over.
Follow Up
Regular checkups are of utmost importance following treatment of thyroid cancer for fear of return of the cancer. Blood tests, imaging will have to be done routinely as per the directions of the doctor. The side effects of the cancer treatments are searched for. Imaging modalities may be an ultrasound scan, PET scan, CT scan or MRI scan.
Treatment using external beam radiation and radioactive iodine may make the patient susceptible to the development of other cancers in the future. Levels of TSH (Thyroid stimulating hormone) and thyroglobulin are monitored in patients who have undergone treatment for papillary or follicular cancers. Thyroglobulin is what thyroid hormone is stored as in the gland. Thus if the whole gland has been removed in a surgery there shouldn’t be any thyroglobulin in blood.










