- Primary Sclerosing Cholangitis – Diagnosis, Prognosis and Management - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3692584/)
- Primary Sclerosing Cholangitis – Diagnosis, Prognosis and Management - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3692584/)
- About Primary Sclerosing Cholangitis - (https://www.ncbi.nlm.nih.gov/books/NBK537181/)
- Recurrence of primary sclerosing cholangitis after liver transplantation – analysing the European Liver Transplant Registry and beyond - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8456806/)
- Autoantibodies in primary sclerosing cholangitis - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2721433/)
- Primary sclerosing cholangitis and ulcerative colitis: evidence for increased neoplastic potential - (https://pubmed.ncbi.nlm.nih.gov/7590655/)
- Primary Sclerosing Cholangitis - (https://my.clevelandclinic.org/health/diseases/23569-primary-sclerosing-cholangitis)
- Neonatal cholestasis due to primary sclerosing cholangitis - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5353830/)
- Cholangitis: Diagnosis, Treatment and Prognosis - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5719198/)
- HLA haplotypes in primary sclerosing cholangitis patients of admixed and non-European ancestry - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7359736/)
- Secondary Sclerosing Cholangitis in Critically Ill Patients: An Underdiagnosed Entity - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7113589/)
- Recurrence of primary sclerosing cholangitis after liver transplantation – analysing the European Liver Transplant Registry and beyond - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8456806/)
- Primary Sclerosing Cholangitis and Inflammatory Bowel Disease: A Review - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9240248/)
- Hepatic sarcoidosis resembling primary sclerosing cholangitis - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8424844/)
- Senescence and tumor suppression - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5730862/)
- Sclerosing Cholangitis: Clinicopathologic Features, Imaging Spectrum, and Systemic Approach to Differential Diagnosis - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4720808/)
- Endoscopic Retrograde Cholangiopancreatography (ERCP) - (https://www.niddk.nih.gov/health-information/diagnostic-tests/endoscopic-retrograde- cholangiopancreatography)
- Liver Function Tests - (https://www.ncbi.nlm.nih.gov/books/NBK482489/)
- Primary sclerosing cholangitis: diagnostic and management challenges - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5680897/)
- Primary Sclerosing Cholangitis: Current and Future Management Strategies - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3652489/)
- A Congenital Choledochal Cyst in an Adolescent: A Unique Case Report and the Role Liver-Specific Contrast Agents in the Diagnosis of Challenging Cases - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9126481/)
- Ursodeoxycholic Acid - (https://www.ncbi.nlm.nih.gov/books/NBK545303/)
- Severe Biliary Stricture Dilation Using the Soehendra Stent Retriever with a Short-Type Balloon Enteroscope in Patients with Surgically Altered Anatomies - (https://pubmed.ncbi.nlm.nih.gov/30284198/)
- The Potentiality of Herbal Remedies in Primary Sclerosing Cholangitis: From In Vitro to Clinical Studies - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7298067/)
- Eating, Diet, & Nutrition for Primary Sclerosing Cholangitis - (https://www.niddk.nih.gov/health-information/liver-disease/primary-sclerosing-cholangitis/eating-diet-nutrition)
- Primary sclerosing cholangitis - (https://pubmed.ncbi.nlm.nih.gov/18701947/)
- Survival and Complication of Liver Transplantation in Infants: A Systematic Review and Meta-Analysis - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8116516/)
About
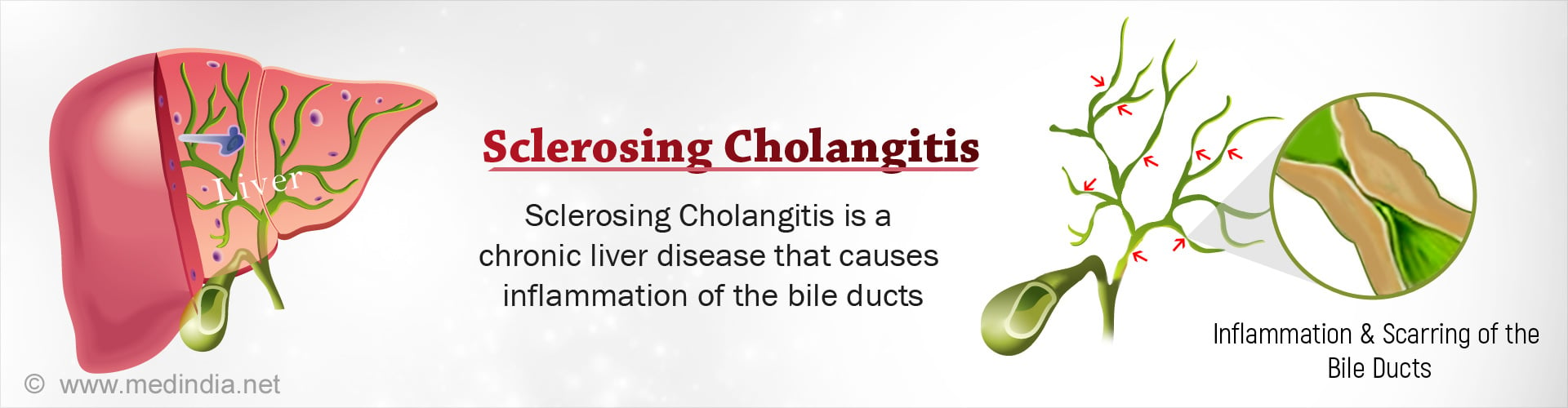
Sclerosing cholangitis involves inflammation of bile ducts, either within the liver or outside the liver. Thus, the flow of bile from the liver to the intestine may be obstructed. The bile accumulates in the liver causing liver damage. Patient may die due to complications like liver failure, bleeding or cancer(1✔ ✔Trusted Source
Primary Sclerosing Cholangitis – Diagnosis, Prognosis and Management
Go to source).
Sclerosing cholangitis (SC) is a chronic and progressive cholestatic liver disorder with an unknown aetiology. Inflammation, fibrosis, and stricturing of intrahepatic and/or extrahepatic biliary ducts characterize SC. It is usually a progressive disorder that can lead to cholestasis and liver failure(2✔ ✔Trusted Source
About Primary Sclerosing Cholangitis
Go to source).
A large number of autoantibodies have been detected in primary sclerosing cholangitis (PSC) patients, but the specificity of these antibodies is usually low, and the frequencies differ between different studies. The presence of autoantibodies in PSC may be because of a nonspecific dysregulation of the immune system, but the literature in PSC points to the possible presence of specific antibody targets in the biliary epithelium and in neutrophil granulocytes(3✔ ✔Trusted Source
Autoantibodies in primary sclerosing cholangitis
Go to source).
SC often affects men in their forties, especially those also suffering from inflammatory bowel diseases like ulcerative colitis.
In addition, bile duct stones, surgery, parasites or drugs are responsible for some cases of sclerosing cholangitis.
Sclerosing cholangitis vs Biliary cholangitis
Primary biliary cholangitis (PBC) and Primary sclerosing cholangtiis (PSC) are both progressive bile duct-related liver diseases, with similar symptoms and effects. Both diseases cause the gradual deterioration of the bile ducts. Destruction and scarring in the bile ducts cause them to narrow and the flow of bile to stall.
The primary differences of PBC and PSC are(4✔ ✔Trusted Source
Primary Sclerosing Cholangitis
Go to source):
- PBC only affects the bile ducts within the liver (intrahepatic), while PSC can affect the bile ducts inside or outside of the liver (extrahepatic).
- PBC is more predominant in people assigned female at birth, by a ratio of 10:1. PSC is more predominant in people assigned male at birth, by a ratio of 2:1.
- PSC is highly associated with preexisting inflammatory bowel disease(80%), while PBC is not.
- PSC is associated with an increased risk of developing bile duct cancer, while PBC is not.
- PBC treatment involves using ursodeoxycholic acid (UDCA) to slow its progression. PSC currently has no medical treatment.
What is Neonatal cholangitis:
Neonatal sclerosing cholangitis (NSC) is a rare autosomal recessive condition., It closely resembles biliary atresia and must be distinguished using biliary imaging(5✔ ✔Trusted Source
Neonatal cholestasis due to primary sclerosing cholangitis
Go to source).
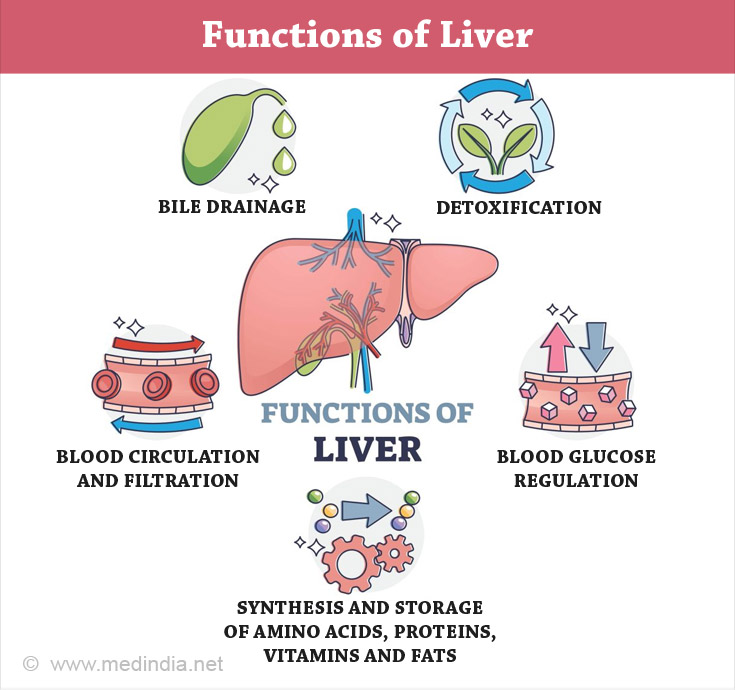
Brief Overview of Liver Structure and Function
The liver consists of two parts, the left lobe and a much larger right lobe. It produces a juice called bile that helps in digestion of fat from food.
Bile travels through a number of small channels within the liver called intra-hepatic bile ducts. These ducts eventually emerge from the liver into two bigger channels, the left and right hepatic ducts. Together they form the common hepatic duct.
The common hepatic duct in turn joins the cystic duct coming from the gall bladder to form the common bile duct.
The gall bladder normally stores the excessive bile produced by the liver. The common bile duct finally opens into the first part of the intestine.
What are the Types of Sclerosing Cholangitis?
Sclerosing cholangitis is of two types, namely(6✔ ✔Trusted Source
Cholangitis: Diagnosis, Treatment and Prognosis
Go to source)
- Primary sclerosing cholangitis
- Secondary sclerosing cholangitis
1. Primary sclerosing cholangitis (PSC) is a chronic liver condition characterized by inflammation and scarring of bile ducts within and outside of the liver. Inflammation leads to the narrowing of some portions of the bile ducts.
The cause of PSC is not known (idiopathic). It could be due to a combination of genetic and environmental factors.
Specific variations of genes called the Human Leukocyte Allele (HLA) complex occur in persons with PSC(7✔ ✔Trusted Source
HLA haplotypes in primary sclerosing cholangitis patients of admixed and non-European ancestry
Go to source). The HLA complex helps the immune system differentiate the body’s own proteins from foreign ones. Variations in the HLA complex can deregulate the immune system causing inflammation of the bile ducts.
2. Secondary Sclerosing Cholangitis (SSC) is a similar condition where the bile ducts are inflamed, leading to scarring and narrowing of the ducts. The causes are usually identifiable like long-term biliary obstruction, infections and inflammation(8✔ ✔Trusted Source
Secondary Sclerosing Cholangitis in Critically Ill Patients: An Underdiagnosed Entity
Go to source).
It results in biliary cirrhosis.
Facts and Statistics of Sclerosing Cholangitis
- It is estimated that 32,000 people in the U.S.A have PSC.
- PSC tends to affect males to females in a 2-3:1 ratio.
- The average life expectancy after diagnosis is between 10 and 20 years. A new lease on life can be offered by a liver transplant. However, in 15% to 20% of cases, PSC can return after a liver transplant. When this happens, the new liver may fail. The average life expectancy in this case is about nine months(4✔ ✔Trusted Source
Primary Sclerosing Cholangitis
Go to source).
Annual incidence rates in Northern Europe range between 0.41 to 1.2 per 100,000 person-years. Rates are lower in Southern Europe, Asia and Alaska.
- In one of the largest ethnically diverse population-based case-finding study in Northern California on PSC in 2011, a prevalence of 4.03 cases per 100,000 and an incidence of 4.1 per 100,000 person-years were reported.
- The estimated median survival in terms of years from the time of diagnosis until liver transplant or a PSC related death is 21.3 years(9✔ ✔Trusted Source
Recurrence of primary sclerosing cholangitis after liver transplantation – analysing the European Liver Transplant Registry and beyond
Go to source). - It presents itself during the 4thor 5th decade of life at approximately 42 years.
- 75% of people with PSC also have
Inflammatory Bowel Disease (IBD)(10✔ ✔Trusted Source .
Primary Sclerosing Cholangitis and Inflammatory Bowel Disease: A Review
Go to source) - The lifetime risk of patients with PSC to develop bile duct cancer is 10-15%.
- PSC is the cause of 5% of the liver transplants done in the U.S.
What are the Causes of Sclerosing Cholangitis?
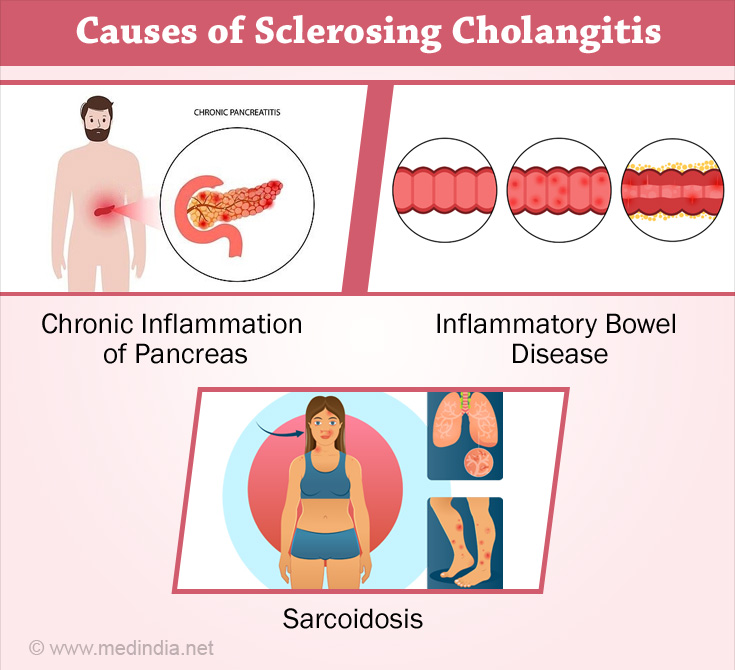
- The cause of Primary Sclerosing Cholangitis (PSC) is primarily unknown.
It occurs in people who also have:
- Autoimmune diseases. Patient who have PSC show the presence of certain antibodies in the blood although the disease is not an auto-immune one.
- Chronic inflammation of the pancreas.
- Inflammatory bowel diseaseslike Ulcerative Colitis (UC) and Crohn's disease(11✔ ✔Trusted Source
Primary sclerosing cholangitis and ulcerative colitis: evidence for increased neoplastic potential
Go to source), Sarcoidosis, a disease that causes inflammation in various parts of the body(12✔ ✔Trusted Source
Hepatic sarcoidosis resembling primary sclerosing cholangitis
Go to source).
Other causes that are yet to be proved are:
- Certain types of Gut bacteria.
- A process called "cellular senescence" that is both tumor suppressive and pro-carcinogenic that is involved in how PSC occurs(13✔ ✔Trusted Source
Senescence and tumor suppression
Go to source).
Conditions that cause secondary sclerotic cholangitis include(2✔ ✔Trusted Source
About Primary Sclerosing Cholangitis
Go to source):
- Stones in the bile ducts (Choledocolithiasis)
- Cancer of the bile ducts inside and outside the liver, gall bladder cancer liver and prostate gland cancers.
- Surgical trauma causing damage to the bile ducts.
- Ischemic causes like damage to the blood supply of the bile ducts.
- Infectious causes like presence of microorganisms in the bile ducts - examples are parasites like cryptosporidium, viruses like cytomegalovirus and fungi like candida. These agents cause direct injury to the biliary cells.
- Disorders of the bile ducts present from birth.
- Toxic causes like chemical agents or drugs (formaldehyde and silver nitrate (0.5%) that are used to kill cysts.
- Infections of the liver and gallbladder
- Immune-induced inflammation (cholangitis) or disease (cholangiopathy) of the bile duct - caused due to excess of eosinophils or mast cells (types of white blood cells), increase in Immunoglobulin G4-positive plasma cells that occurs with autoimmune pancreatitis (inflammation of the pancreas).
- Pancreatic disorders like autoimmune and chronic inflammation of pancreas.
- Intra-arterial chemotherapy where the drugs are administered directly to the tumor so that healthy tissues are not affected.
- Chronic obstruction of the bile ducts causing thickening of its walls resulting in recurrent inflammation
- Sclerosing Cholangitis in critically ill patients (called SC-CIP) like those with cancer.
What are the Symptoms and Signs of Sclerosing Cholangitis?
Many patients with primary sclerosing cholangitis may not experience any symptoms initially but a substantial proportion may exhibit the following symptoms and signs(2✔ ✔Trusted Source
About Primary Sclerosing Cholangitis
Go to source):
- Fever, chills and abdominal pain (right, upper quadrant) due to bile infection.
- Fatigue often present in liver disease. Itching or Pruritus which may be severe. Jaundice - yellowing of the white portions of the eyes and skin.
As the disease progresses symptoms could include:
- Loss of appetite and weight loss
- Fluid in the abdomen
- Confusion
- Intestinal bleeding due to enlarged veins.
- Episodes of acute infection of bile ducts, sometimes life-threatening.
- Dark urine due to the presence of excess bilirubin.
- Malabsorption of fat due to inadequate bile reaching the small intestine and decreased levels of fat-soluble vitamins.
- The patient may pass excessive fat in the stools leading to bulky, foul smelling stools.
- Increased pressure in the veins of the liver system (portal hypertension) due to compression by the damaged bile ducts inside.
- Enlarged liver due to portal hypertension.
- Physical signs: The skin may show darkening and scratch marks due to itching. The patient’s abdomen may appear bloated in severe cases due to accumulation of fluid (ascites).
Secondary Sclerosing Cholangitis also has no initial symptoms except for abnormal liver function test results.
As the disease progresses, there is decreased bile flow. Clinical symptoms are jaundice, itching and right upper abdominal discomfort.
Ascending liver infection is seen in mostly all cases with SSC as also recurrent episodes of bacterial bile duct.
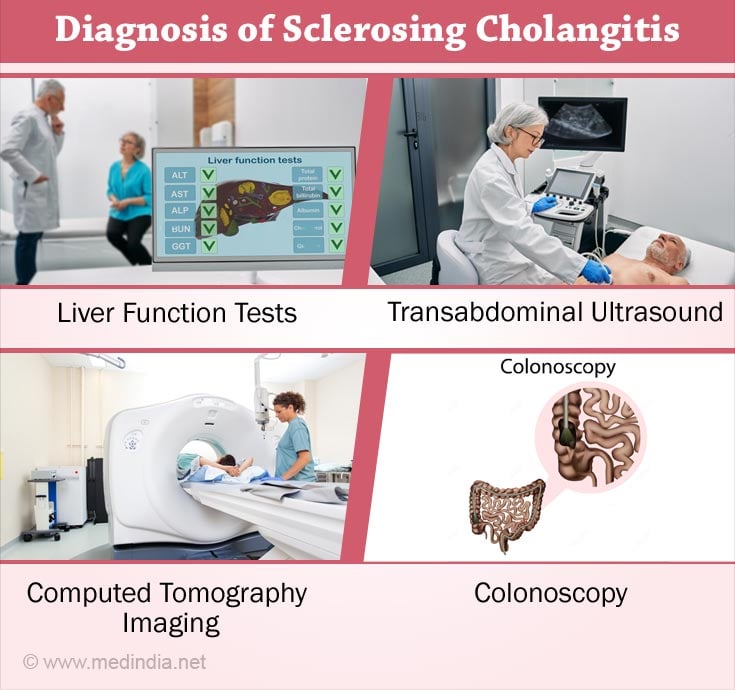
How is Sclerosing Cholangitis Diagnosed?
Diagnosis of PSC is made incidentally when liver function tests are done for decreased bile flow or because it usually occurs along with ulcerative colitis.
A diagnosis of PSC is based on the presence of bile duct scars using imaging studies like endoscopic retrograde cholangiography and magnetic resonance cholangiography(14✔ ✔Trusted Source
Sclerosing Cholangitis: Clinicopathologic Features, Imaging Spectrum, and Systemic Approach to Differential Diagnosis
Go to source).
1. Cholangiography: Cholangiography is a procedure in which contrast agent is introduced into the bile ducts. The passage of the contrast agent through the ducts is studied using x-rays or scans. Two types of cholangiography are used, endoscopic retrograde cholangiography and magnetic resonance cholangiography.
- In endoscopic retrograde cholangiography (ERC), the doctor introduces a tube called an endoscope through the mouth till it reaches the duodenum and visualizes the bile duct opening. A small plastic tube is inserted through the endoscope into the bile duct. Contrast agent is then injected into the bile ducts and x-rays taken to look for any abnormalities in the bile ducts(15✔ ✔Trusted Source
Endoscopic Retrograde Cholangiopancreatography (ERCP)
Go to source).
This is an invasive technique that can produce complications like pancreatitis and bacterial cholangitis.
- Magnetic resonance cholangiography (MRC) is a comparatively simpler test and is preferred by many doctors. It is a non-invasive imaging technique to visualize the biliary ducts. One drawback is that early changes in PSC might not be detected as well as in ERC.
2. Liver Function Tests (LFTs): LFTs are blood tests used to check if the liver is functioning properly. They are done if the cholangiography shows changes in the bile ducts and if secondary causes of the disease have been eliminated(16✔ ✔Trusted Source
Liver Function Tests
Go to source).
Certain enzymes like alkaline phosphatase, serum aminotransferase and/or gamma - glutamyl transpeptidase (GTT) are increased in patients with primary sclerosing cholangitis (PSC). However, their levels may be high in other liver conditions as well.
Serum bilirubin levels are surprisingly normal in most patients at the time of diagnosis. IgG serum levels are 1.5 times more in approximately 60% of the patients.
3. Liver Biopsy: Biopsy of the liver may help in the diagnosis of sclerosing cholangitis(17✔ ✔Trusted Source
Primary sclerosing cholangitis: diagnostic and management challenges
Go to source). Although early changes cannot be seen, it could indicate some kind of biliary disease.
In the case of a large duct PSC, a biopsy need not be done if the cholangiogram is abnormal. It is however useful in small duct PSC.
Small duct PSC is a disease variant that has similar symptoms of PSC but shows the presence of normal bile ducts on cholangiography.
Distinguishing primary from SSC is difficult:
- Many types of SSC like those caused by gallstones, surgical trauma, intra-arterial chemotherapy, immune-related and infection-induced cholangitis all show similar clinical and cholangiographic symptoms.
- Also, some PSC patients might have undergone a bile duct surgery or have gallstones or have bile duct cancer.
Hence, clinical history, distribution of cholangiographic findings and whether IBD is present or not will determine if an abnormal cholangiogram is due to primary or secondary sclerosing cholangitis.
Other tests that can be done are:
4. Serology: A variety of autoantibodies at low prevalence rates can be detected in the serum of PSC patients. This may indicate immune regulation.
5. Tran-abdominal ultrasound identifies gallbladder abnormalities like wall thickening, enlargement, stones, decreased bile flow and mass lesions in 41% of the patients. Noting bile duct wall thickening is rarer(18✔ ✔Trusted Source
Primary Sclerosing Cholangitis: Current and Future Management Strategies
Go to source).
6. Computed Tomography (CT) imaging of the upper abdomen can detect thickening and inflammation of the bile ducts and document splenomegaly, fluid and lesions that are signs of portal hypertension.
7. Imaging tests to evaluate bone density due to decreased Vitamin D.
8. A colonoscopy to evaluate colitis or inflammation of the colon. Colonoscopy has to be repeated yearly to screen for colon cancer.
For Secondary Sclerosing Cholangitis (SSC), ultrasonography is performed after highly elevated serum levels of alkaline phosphatase and α-glutamyl transferase are obtained on the Liver Function Test results.
If SSC has been caused by chronic biliary obstruction, ultrasonography will detect gallstones, dilation of the bile duct or hepatic abscess. Ultrasonography is not useful if biliary obstruction is not the cause.
The "gold standard" procedure therefore remains endoscopic retrograde cholangiopancreatography (ERCP) (otherwise known as ECR) that will reveal the bile ducts to have a beaded appearance(19✔ ✔Trusted Source
A Congenital Choledochal Cyst in an Adolescent: A Unique Case Report and the Role Liver-Specific Contrast Agents in the Diagnosis of Challenging Cases
Go to source). This is caused due to primary sclerosing cholangitis like biliary lesions, with narrowed and dilated intervening segments of ducts.
Magnetic resonance cholangiopancreatography (MRCP) (otherwise known as MRC) is less invasive but is not useful in early detection of SSC.
What is the Treatment for Sclerosing Cholangitis?
Focus has to be on managing severe itching, other complications and periodic monitoring of the extent of liver damage. Medications have not been shown to reverse liver damage. There is currently no effective new treatment for sclerosing cholangitis.
- Antihistamines - diphenhydramine and loratidine can work by reducing itching but may worsen liver disease symptoms like dry eyes and mouth.
- Drugs like cholestyramine work by reducing levels of bile acids in the blood and thus reduce itching.
- Rifampicin, an antibacterial drug that may work by blocking the brain’s response to the chemicals in circulation causing itching.
- Opioid antagonist drug like naltrexone reduces itching due to liver disease.
- A drug, ursodeoxycholic acid UDCA may be useful in the early stages to increase bile flow and to reduce biliary inflammation. It is a naturally occurring bile acid(20✔ ✔Trusted Source
Ursodeoxycholic Acid
Go to source). - Fat-soluble vitamin supplements like D, A, E and K that have been lost be are replaced as tablets or intravenous infusion.
- Calcium and Vitamin D supplements if the disease has weakened the bones.
- Repeated courses of antibioticsto treat infections due to stagnant bile in narrow and blocked ducts maybe required. Antibiotics also need to be taken before an endoscopy or surgery.
- Medicines to suppress the immune system like prednisone, azathioprine, cyclosporine and methotrexate maybe tried in some cases.
Surgery maybe required to treat sclerosing cholangitis.
Balloon dilation: Strictures in the bile ducts may be dilated during endoscopic retrograde cholangiography procedure(21✔ ✔Trusted Source
Severe Biliary Stricture Dilation Using the Soehendra Stent Retriever with a Short-Type Balloon Enteroscope in Patients with Surgically Altered Anatomies
Go to source).
A tube with a deflated balloon is introduced into the liver through the endoscope until it reaches the narrow part of the bile duct.
In this position, the balloon is inflated, thus resulting in widening of the narrowed part. It opens up the blockages in the larger bile ducts outside the liver.
Stent placement: Stents or small tubes may be placed in the bile ducts to relieve the obstruction and to hold the duct open. The procedure is performed using an endoscope and attached instruments. However, the stents could result in increased chances of infection.
Procto-colectomy or the removal of colon and rectum if primary sclerosing cholangitis is present along with ulcerative colitis. Complications like gall bladder stones and polyps may necessitate removal of the gall bladder.
Liver Transplant: Liver transplantation helps to improve survival in patients with primary sclerosing cholangitis having liver failure or complications(2✔ ✔Trusted Source
About Primary Sclerosing Cholangitis
Go to source). The diseased liver is taken out and replaced with a healthy liver from a donor.
Some people (25%) however may develop sclerosing cholangitis in the transplanted liver.
Reconstructive procedures like choledochoduodenostomy and choledochojejunostomy where the bile duct is attached to the duodenum and jejunum respectively to alleviate symptoms.
Natural Treatment for Sclerosing Cholangitis
Silybum marianum
Silybum marianum, also known as milk thisle has long been utilised in the treatment of biliary and liver ailments.
Salvia miltiorrhiza
Salvia miltiorrhiza is a well-known traditional Chinese remedy that has been shown to reduce liver fibrosis.
Curcuma longa
Curcuma longa (Turmeric) has been used for centuries for its anti-inflammatory properties in both Ayurvedic and Chinese medicine.
Quercetin
Quercetin is a natural flavonoid found in many vegetables and fruits belonging to the Apiaceae family that has been shown to reduce liver fibrosis(22✔ ✔Trusted Source
The Potentiality of Herbal Remedies in Primary Sclerosing Cholangitis: From In Vitro to Clinical Studies
Go to source).
Dietary restrictions
People suffering from primary sclerosing cholangitis (PSC) should eat a healthy, well-balanced diet. Nutrition is critical at all stages of PSC, including cirrhosis, to help the liver function properly and manage complications(23✔ ✔Trusted Source
Eating, Diet, & Nutrition for Primary Sclerosing Cholangitis
Go to source).
What are the Complications of Sclerosing Cholangitis?
Complications of sclerosing cholangitis occur due to vitamin deficiency and accumulation of bile in the liver(24✔ ✔Trusted Source
Primary sclerosing cholangitis
Go to source).
- Jaundice due to complete blockage of the bile ducts.
- Cholangitis or inflammation of the bile duct system.
- Vitamin Deficiency: Bile secreted by the liver helps in absorption of certain vitamins i.e. A, D, E and K. Absence of bile in the intestines in sclerosing cholangitis causes loss of these vitamins in the stools leading to vitamin deficiency.
- Osteoporosis or thinning of the bones due to vitamin D leads deficiency
- Cholangiocarcinoma or cancer of the bile ducts. Cholangiocarcinoma occurs in 10 to 15% of patients with PSG. The cancer could spread to other parts of the body as well. The patient is also at an increased risk for developing cancer of the pancreas, gall bladder and colon.
- The bile ducts may be narrowed resulting in the formation of strictures and strictures can obstruct the flow of bile.
- The bile ducts could be more prone to bacterial infection.
- Gallbladder stones and polyps may form due to accumulation of bile in the gall bladder.
- Cirrhosis or severe scarring of the liver. Cirrhosis could progress to an advanced stage leading to liver failure.
- Enlargement of esophageal veins leads to bursting and bleeding. Cirrhosis causes shortage of blood flow in the liver leading to more blood flow or enlarged veins in esophagus.
- High pressure in the portal venous system of the liver could result in a condition called portal hypertension. This could result in bleeding at the lower end of the food pipe (esophagus).
- Alteration or disturbance of mental status called hepatic encephalopathy caused by liver dysfunction that shunts blood away from the liver.
- Gallbladder cancer.
- Colon cancer when PSC occurs along with Inflammatory Bowel disorder.
What is the Prognosis of PSC?
The average time taken from the point of diagnosis of primary sclerosing cholangitis until liver transplant or death is around 21 years. The disease worsens progressively and could lead to cholangiocarcinoma, liver failure, infections of bile ducts that keep returning, persistent jaundice or bleeding.
Due to the progressive nature of the disease, 40% of patients will ultimately require a liver transplant.
The one-year survival rate after a liver transplant is approximately 85% and the five-year rate is 72%(25✔ ✔Trusted Source
Survival and Complication of Liver Transplantation in Infants: A Systematic Review and Meta-Analysis
Go to source).