- Grogan M, Redfield MM, Bailey KR, Reeder GS, Gersh RJ, Edwards WD, Rodeheffer RJ. Long-term outcome of patients with biopsy-proved myocarditis: comparison with idiopathic dilated cardiomyopathy. J Am Coll Cardiol. 1995;26:80–84.
- Clinicopathologic description of myocarditis. - (http://www.ncbi.nlm.nih.gov/pubmed/1960305)
- Myocarditis - (https://www.ahajournals.org/doi/full/10.1161/circulationaha.105.584532)
- Cooper LT, Berry GJ, Shabetai R, for the Multicenter Giant Cell Myocarditis Study Group Investigators. Idiopathic giant-cell myocarditis: natural history and treatment. N Engl J Med. 1997;336:1860–1866. - (https://www.ahajournals.org/doi/full/10.1161/circulationaha.105.584532)
What is Myocarditis?
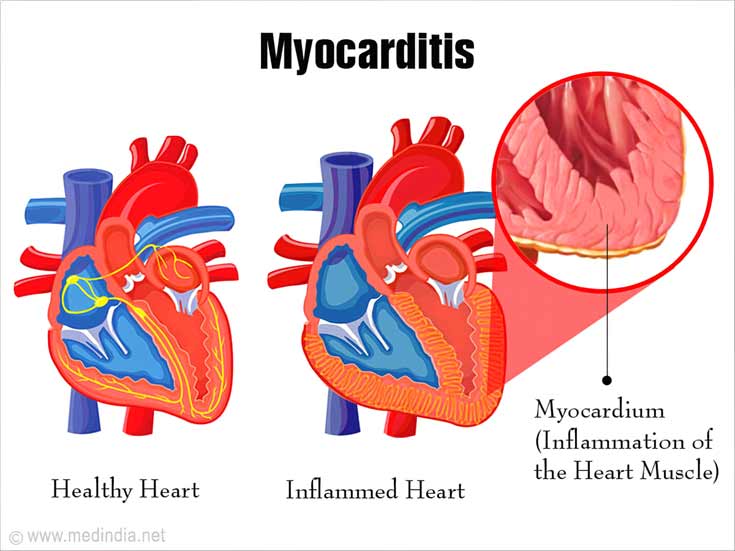
Myocarditis is an inflammation of the middle layer of the heart. Structurally, the heart has three layers, which are the outer protective layer called the pericardium, the middle muscle layer called the myocardium and the inner valve layer called the endocardium. When there is an infection of the body by some viruses, or rarely some bacteria or parasites, or when there is a state of inflammation in the body due to certain diseases, the muscle layer of the heart might be attacked by the body’s own immune cells. This results in myocarditis. Myocarditis presents in various nonspecific ways and is difficult to diagnose. It is usually a self-limiting disease with minimal residual damage, but it may cause serious illness in certain individuals.
What are the Types of Myocarditis?
There are several systems of classification of myocarditis, based on the causative factor, the clinical status and the pathological characteristics.
Lieberman’s clinicopathological classification
- Fulminant myocarditis – severe disease following viral infection, leading to sudden compromise of organ systems
- Acute myocarditis – patients present with heart dysfunction, which may respond to treatment
- Chronic active myocarditis – these patients initially respond to treatment, but then relapse and finally develop heart dysfunction
- Chronic persistent myocarditis – they have persistent inflammation, but minimal to no heart dysfunction
Pathological classification
- Lymphocytic – viral, autoimmune
- Eosinophilic – hypersensitivity myocarditis
- Granulomatous – giant cell myocarditis
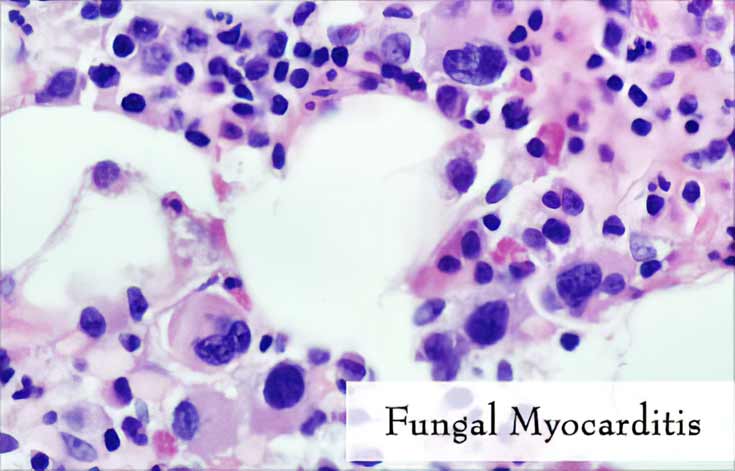
- Neutrophilic – bacterial, fungal myocarditis
- Reperfusion type/contraction band necrosis – due to certain drugs
Etiological classification
- Infectious
- Post viral autoimmune mediated
- Autoimmune – mediated
- Drug associated
What are the Causes of Myocarditis?
The causes of myocarditis are numerous and can be grouped into:
1. Infectious
- Viral
- Adenovirus
- Coxsackie virus
- Hepatitis C Virus
- HIV
- Parvovirus B19
- Enterovirus
- Hepatitis A virus
- Epstein Barr virus
- Dengue fever
- Rubella
- Yellow fever
- Rabies virus
- Polio
- Rubella
- Bacterial
- Tuberculosis
- Diphtheria
- Streptococcus
- Mycoplasma
- Treponema pallidum (Syphilis)
- Lyme disease
- Fungal
- Aspergillus
- Candida
- Histoplasma
- Parasites
- Chagas disease (Trypanosomiasis)
- Schistosomiasis
2. Drug induced
- Direct toxic effect
- Anticancer drugs – anthracyclines, 5-fluorouracil, cyclophosphamide
- Interleukin 2
- Trastuzumab
- Cocaine
- Amphetamines
- Hypersensitivity reactions
- Cephalosporin group of antibiotics
- Digoxin
- Diuretics
- Dobutamine
3. Immunological
- Churg-Strauss Syndrome
- Wegener’s granulomatosis
- Inflammatory Bowel Disease
- Giant cell myocarditis – it is a chronic disease the cause of which is not known, and which can only be diagnosed by biopsy of the heart. It is characterized by abnormal giant cells in the heart. It is often fatal.
- Sarcoidosis
- Diabetes mellitus Type I
- Systemic Lupus Erythematosus
- Scleroderma
- Myasthenia gravis
- Polymyositis
- Takayasu’s arteritis
- Kawasaki disease

The most common cause of myocarditis is viral infections. Viruses may both directly damage the muscle layer of the heart or may incite the immune system of the body to target the heart muscle.
Even in children, viruses remain the most common cause of myocarditis. Rarely, bacteria can cause myocarditis, prominent among them being Corynebacterium diphtheriae, the bacterium that causes diphtheria. Other common causes of myocarditis in children are allergic response to antibiotics including penicillin and the cephalosporin group, and inflammatory disorders that manifest in childhood, such as Kawasaki disease.
What are the Symptoms and Signs of Myocarditis?
The presentation of myocarditis is very variable. Some patients may not have any symptoms at all, with only minor ECG changes, while some patients may develop severe heart failure and even sudden death. The most common complaints are:
- Fatigue
- Chest pain
- Fever
- Shortness of breath
- Palpitation – a feeling of a racing heart
- Symptoms of the viral infection – diarrhea, vomiting, joint pain, runny nose etc.
- Symptoms in new-borns may include:
- Poor weight gain
- Feeding difficulties
- Fever
- Restlessness
- Low urine output (in severe disease)
- Cool hands and feet
- Rapid breathing
- Symptoms in children include:
- Pain in the abdomen
- Chest pain
- Cough
- Fatigue

Some individuals may develop symptoms mimicking a myocardial infarction (heart attack).
If affected individuals develop severe heart disease, they may experience breathlessness, swelling of the feet, low urine output, a feeling of tightness in the chest and an inability to maintain oxygenation of the blood. Symptoms of fulminant myocarditis have an abrupt onset and usually progress to severe heart dysfunction within 3 days.
Clinical examination may reveal an increased heart rate, a soft first heart sound and an S4 gallop. Associated findings of the cause of myocarditis may be present, such as joint tenderness in viral infections and signs of vasculitis etc. Once heart dysfunction sets in, signs of cardiac failure may manifest, such as pulmonary edema (fluid accumulation in the lungs), peripheral oedema, hypoxemia, pulsus alternans, etc. Patients may be hypotensive (having low blood pressure), which is a dangerous sign, and may require intravenous medications to keep their blood pressure in the normal range.
Complications
- Heart failure
- Pulmonary oedema
- Cardiogenic shock
- Arrhythmia
- Dilated cardiomyopathy
How to Diagnose Myocarditis?
As the presentation of myocarditis might be vague, investigations are needed to confirm the diagnosis. These include:
ECG
- An electrocardiogram is the most basic test done for the diagnosis of myocarditis
- It can show changes similar to those of a heart attack, or it may reveal some complications such as arrhythmias and heart blocks.
Blood tests
- Routine investigations such as complete blood count, which will likely show a raised WBC count
- Cardiac markers such as Troponin I and Troponin T, which are elevated when there is damage to the heart muscle
- Markers of inflammation such as ESR and CRP may be raised
Chest X ray
- Chest X ray is usually normal, but it may show changes if there are complications such as heart failure or if there is associated pericarditis.
Imaging studies of the heart
- Echocardiography is recommended for all patients who are suspected to have myocarditis
- Cardiac MRI is used to differentiate between heart attack (myocardial infarction) and myocarditis
- Nuclear imaging with gallium67 or indium111-labeled anti-myosin antibodies
Investigations to reveal the cause
- Serological tests against viruses, or specific tests to confirm autoimmune diseases may be done based on clinical suspicion.
Biopsy
- Endomyocardial biopsy, that is taking a piece of the heart muscle and then look for signs of inflammation, is the most specific test for diagnosis.
What are the Treatment for Myocarditis?
Viral myocarditis
- The first line of treatment is supportive care. This includes constant monitoring and medications to treat the underlying cause, and to prevent complications from occurring.
- There are no specific medications to treat viral myocarditis, but research is underway to test the efficacy of treatments such as interferons.
- Patients with signs of fulminant or acute myocarditis may have to be shifted to the ICU as circulatory collapse can occur.
- Patients with heart failure will have to be managed with medications like diuretics (e.g. furosemide) and vasodilators (e.g. nitro-glycerine infusion).
- Patients who develop arrhythmias (abnormalities in the rhythm of the heart) may need blood thinning medications (anticoagulants) to prevent stroke and pulmonary embolus.
- In patients with severe heart failure, medications such as dobutamine and milrinone and other methods to assist the circulation and respiration may be required..
- In very severe, complicated disease, the circulation of blood may be compromised and the body’s tissues may be devoid of oxygen – a state known as circulatory shock. For individuals in whom this occurs, ventricular assist devices and extracorporeal membrane oxygenation (ECMO) may be required.

Other treatments
- Steroids and immunosuppressants are used in giant cell and eosinophilic myocarditis.
- They may also be helpful when the underlying cause is auto-immune related.
- The ultimate treatment for chronic myocarditis such as giant cell myocarditis which has not responded to steroids and other medications, is heart transplantation.
Prognosis of Myocarditis
The prognosis varies with the type of myocarditis. Many studies have been done to predict the outcome of disease, but no reliable markers are available thus far. Hence predicting a prognosis for an individual patient is quite difficult. But it has been found that patients who have resolution of inflammation in the heart on repeated biopsies have the best prognosis.
Studies done on the outcomes of myocarditis show that mortality rates for biopsy-proven cases reach almost 50% after 5 years. The outcome is significantly worse in patients with giant cell myocarditis, with the 5-year survival rate being 20%. Surprisingly, it has been found that the survival rate is the highest in patients with fulminant myocarditis.
Health Tips
- Never ignore a feeling of tightness or mild pain in the chest. Consult your doctor immediately.
- If you have been diagnosed with an autoimmune condition, always remember to take your medications.
- If you feel lethargic after a cold, and you feel like your heart is racing, consult your doctor.
- Do not take over the counter medications in these situations.