- Depression and Anxiety More Common in Adolescents with Dysmenorrhea - (https://womensmentalhealth.org/posts/depression-and-anxiety-more-common-in-adolescents-with-dysmenorrhea/)
- Know More About Dysmenorrhea - (http://www.aafp.org/afp/2012/0215/p386.html)
- Menstrual cramps Treatment - (http://www.mayoclinic.org/diseases-conditions/menstrual-cramps/basics/treatment/con-20025447)
- Dysmenorrhea - Introduction - (https://en.wikipedia.org/wiki/dysmenorrhea#causes)
What is Dysmenorrhea?
Dysmenorrhea means painful periods. It is the most commonly reported menstrual disorder. Most women suffer mild discomfort and pain in the lower abdomen before and during their periods.
However, for some the discomfort and cramping may be severe enough to disrupt their daily activities and routine for a few days every month.

What are the Types of Dysmenorrhea?
Dysmenorrhea is of two types
- Primary
- Secondary
Primary dysmenorrhea is defined as painful menstruation for which no underlying pelvic pathology can be ascertained.
The pain is usually maximum on the first day of the cycle and then reduces in severity.
Primary dysmenorrhea is generally seen in younger girls soon after they attain menarche.
The symptoms of primary dysmenorrhea generally improve with age and following childbirth.
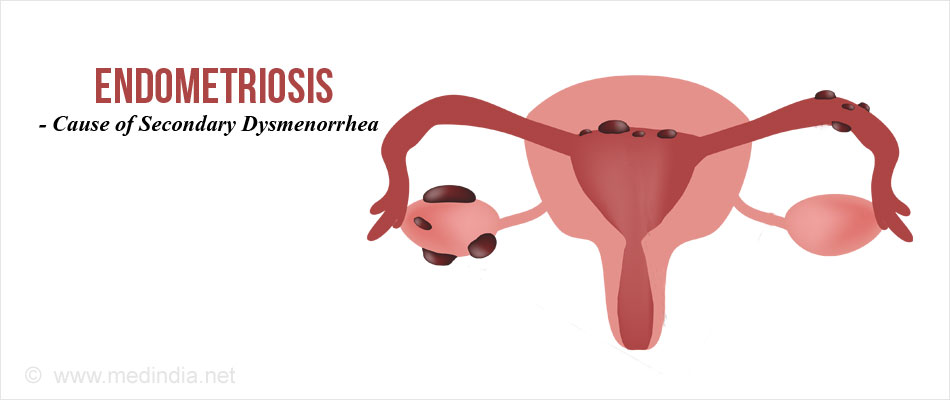
Secondary dysmenorrhea is painful menstruation associated with an underlying pelvic abnormality such as endometriosis, uterine fibroid, or pelvic inflammatory disease (PID).
During each cycle, the pain begins even before the onset of menstrual flow and may continue even after it ends.
Symptoms of secondary dysmenorrhea begin at a later age compared to primary dysmenorrhea. Also the symptoms tend to get worse over time instead of improving.
What are the Symptoms of Dysmenorrhea?
Symptoms of dysmenorrhea include
- Throbbing or cramping pain in the lower abdomen that may be severe
- Dull, constant pain throughout
- Pain that radiates to lower back and thighs
Other associated symptoms
- Diarrhea
- Headaches
- Giddiness
- Nausea

What are the Causes of Dysmenorrhea?
A. Primary Dysmenorrhea
- Chemicals called prostaglandins have been implicated in the pathogenesis of primary dysmenorrhea.
- Prostaglandins are naturally occurring chemicals occurring in the lining of the uterus. The major prostaglandin involved is Prostaglandin F2α.
- Women with primary dysmenorrhea are found to have elevated levels of prostaglandins in their uterus.
- Prostaglandins cause pain and cramps by the following mechanisms
- Contraction of uterine muscle leading to pain
- Cause narrowing of the uterine blood vessels (vasoconstriction), reducing oxygen supply to the uterine tissues causing pain.
- Behavioral and psychological factors are also thought to play a role, though yet to be fully understood.
- A recent study conducted and published by Massachusetts General Hospital (MGH) Center For Women's Mental Health on January 25, 2016 has found a correlation between PMS and dysmenorrhea in adolescence.
- A study published in the J Pediatr Adolesc Gynecol. 2014 Dec;27(6):371-4, and titled ‘Is there a relationship between mood disorders and dysmenorrhea’has concluded that adolescent girls with dysmenorrhea have increased risk of depression and anxiety.
These results are important in emphasizing the importance of a multidisciplinary approach to primary dysmenorrhea follow-up and treatment.
B. Secondary Dysmenorrhea
Prostaglandins may play a role in secondary dysmenorrhea, but an underlying pelvic abnormality is always present. The common causes of secondary dysmenorrhea include:
- Uterine fibroids – benign growths in the wall of the uterus
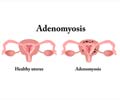
- Adenomyosis - the lining of the uterus occurs abnormally in the muscle layer of the uterus
- Pelvic inflammatory disease (PID) - caused by bacterial infection of the genital tract.
- Cervical stenosis – the opening of the cervix is narrow and hinders the menstrual flow causing pain.
- Endometriosis – when the uterus lining (endometrium) is found in ectopic sites like ovaries, tubes and pelvic wall.
How do you Diagnose Dysmenorrhea?
Primary Dysmenorrhea
No tests are specific to the diagnosis of primary dysmenorrhea. The diagnosis is usually made on the basis of history and clinical findings.
Secondary Dysmenorrhea
Diagnostic studies may be indicated to elucidate the cause of secondary dysmenorrhea.
These include:
- Blood tests to rule out an infectious process in the pelvic organs. These include a Total Count (TC) and a Differential Count (DC).
- Bacteriological tests to rule out sexually transmitted diseases (STD)and pelvic inflammatory disease (PID).
- Urinalysis to exclude urinary tract infection (UTI)
- Abdominal or transvaginal ultrasound to exclude abnormalities in the cervix, uterus, tubes and ovaries.
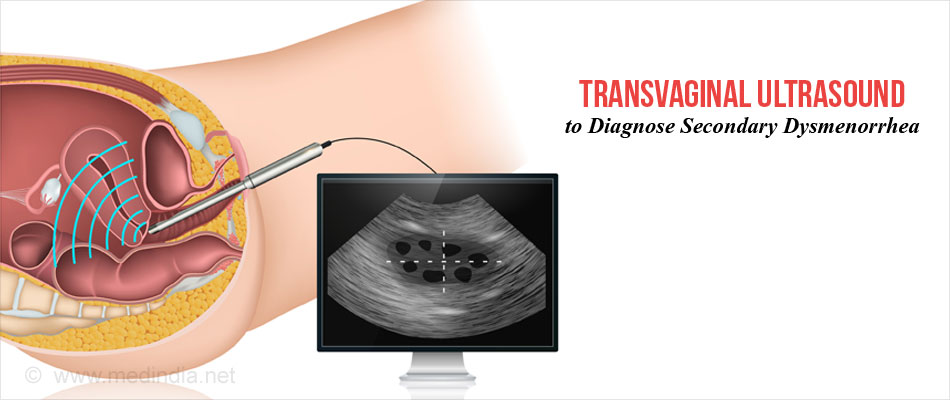
- CT and MRI - They are NOT routine investigations for dysmenorrhea. They may be needed to detect lesions that are missed by other imaging procedures such as ultrasound.
- Rarely a diagnostic laparoscopy may be necessary to survey the pelvic organs and assess any abnormalities like endometriosis.
How do you Treat Dysmenorrhea?
The following modalities of treatment are generally recommended.
A. Pain Relief Medications
- Certain groups of drugs termed Non-Steroidal Anti-inflammatory Drugs (NSAIDs) inhibit the effects of prostaglandins and are effective in the management of dysmenorrhea. They should be taken as soon as the cramps start or the periods begin. They have to be taken for 1-2 days.
- Women with aspirin allergy, asthma, bleeding disorders, stomach disorders (gastritis), ulcers, or liver disease should avoid taking NSAIDs.
- Other drugs that are useful in dysmenorrhea, include aspirin and acetaminophen.
- People who are unable to take NSAIDs may also be prescribed COX-2 inhibitors.
B. Birth Control Pills
Oral contraceptive pills (OCP’s) contain hormones (combination of estrogen and progesterone) that prevent ovulation and reduce the severity of menstrual cramps. They also decrease menstrual flow.- These hormones can also be given as an injection, a skin patch, an implant placed under the skin of arm, a flexible ring inserted into the vagina, or an intrauterine device (IUD).
- OCP’s may be an appropriate choice for patients who do not wish to have children.
Other Drugs and Newer Modalities of Treatment
Many newer drugs and interesting modalities of treatment have been studied in the management of dysmenorrhea. However, more studies have to be conducted for definitive proof of their efficacy.
An article was published in Am Fam Physician. 2012 Feb 15;85(4):386-387 titled ‘Dysmenorrhea’.
This article has taken excerpts from the Clinical Evidence Handbook, published by the BMJ Publishing Group, London, U.K. This study has compared the benefits of various treatments of dysmenorrhea as follows.
| Efficacy | Type of treatment |
| Beneficial | Nonsteroidal anti-inflammatory drugs (other than aspirin) |
| Likely to be beneficial | Aspirin and paracetamol combination Acupressure Behavioral interventions (relaxation) Contraceptives (combined oral) Herbal remedies other than toki-shakuyaku-san Thiamine Topical heat (about 102°F [39°C]) Transcutaneous electrical nerve stimulation (high-frequency stimulation only; effects of low-frequency stimulation remain unclear) |
| Unknown efficacy | Acupuncture Fish oil Magnets Progestogens (intrauterine) Vitamin B12 |
| Unlikely to be beneficial | Spinal manipulation |
| Likely to be ineffective or harmful | Surgical interruption of pelvic nerve pathways |
C. Surgery
- If the menstrual cramps are caused by an underlying disorder, such as endometriosis, cervical stenosis or fibroids, surgery to correct the problem may be necessary to Get rid of the symptoms.
- Surgical removal of the uterus (hysterectomy) also may be an option in women who have completed their family or in those who do not want to have children.

- A surgical procedure called uterine artery embolization (UAE) may be done if uterine fibroids are causing the dysmenorrhea but this is rarely required.
How do you Prevent Dysmenorrhea?
- Lifestyle modification such as stress reduction seems to be helpful
- Stop smoking and alcohol consumption or at least cut it down as much as possible
- Avoid foods such as coffee, tea, oily and spicy foods
- Yoga and Exercise have been shown to give relief to symptoms of dysmenorrhea
- Certain foods can reduce abdominal cramps and may work for some and these include - bananas, wheat germ, sunflower seeds, oats, parsley, salmon, dark chocolate, pineapple seeds, ginger, fenugreek seeds, spinach and green tea