- TMJ (Temporomandibular Joint and Muscle Disorders) - (https://www.nidcr.nih.gov/oralhealth/topics/tmj/tmjdisorders.htm)
- TMJ disorders - (http://www.mayoclinic.org/diseases-conditions/tmj/home/ovc-20209398)
- TMJ - (http://www.mouthhealthy.org/en/az-topics/t/tmj)
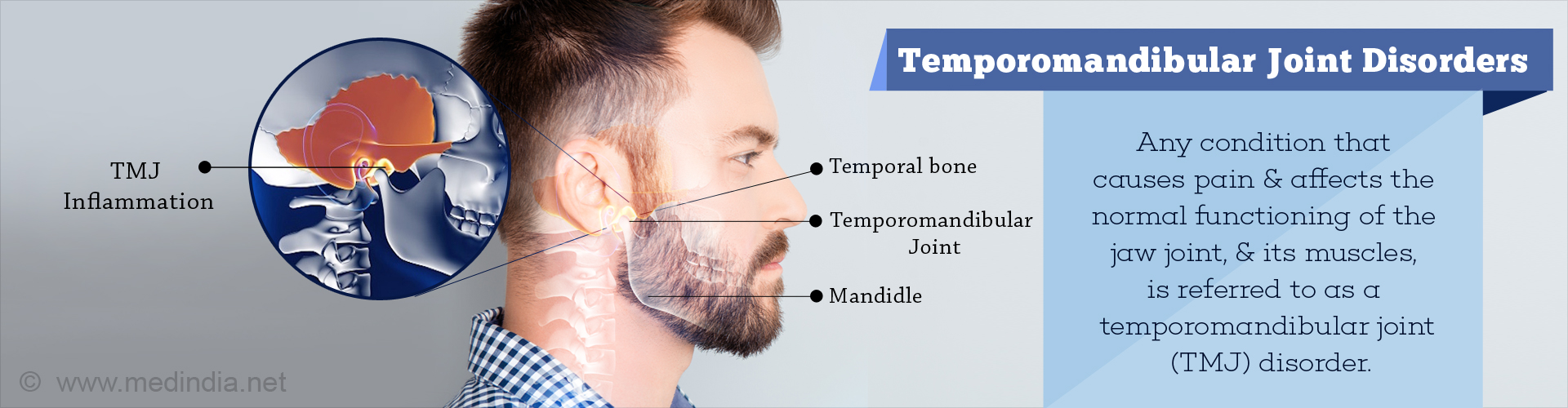
What are Temporomandibular Joint Disorders?
The temporomandibular joint (TMJ) is a hinge joint between the lower jaw (mandible) and the temporal bone of the skull, just in front and below each ear. It is also referred to as the craniomandibular joint.
The movements occurring at the joint include moving the jaw up and down, forwards and backwards, and side to side. The TMJ is thus important for talking, chewing food, swallowing, and even kissing and yawning. The muscles and ligaments that surround the joint allow the smooth and painless movement of the joint.
It is estimated that about 10 million people in the United States alone suffer from some form of temporomandibular joint disorder. For reasons not known, it is more common in women. Persons between 20-40 years of age are commonly affected. TMJ disorders are the second most common reason for orofacial pain, next to toothache.
Generally, symptoms of TMJ disorder are not serious though they cause some discomfort. When they are severe, specialist treatment may be necessary.
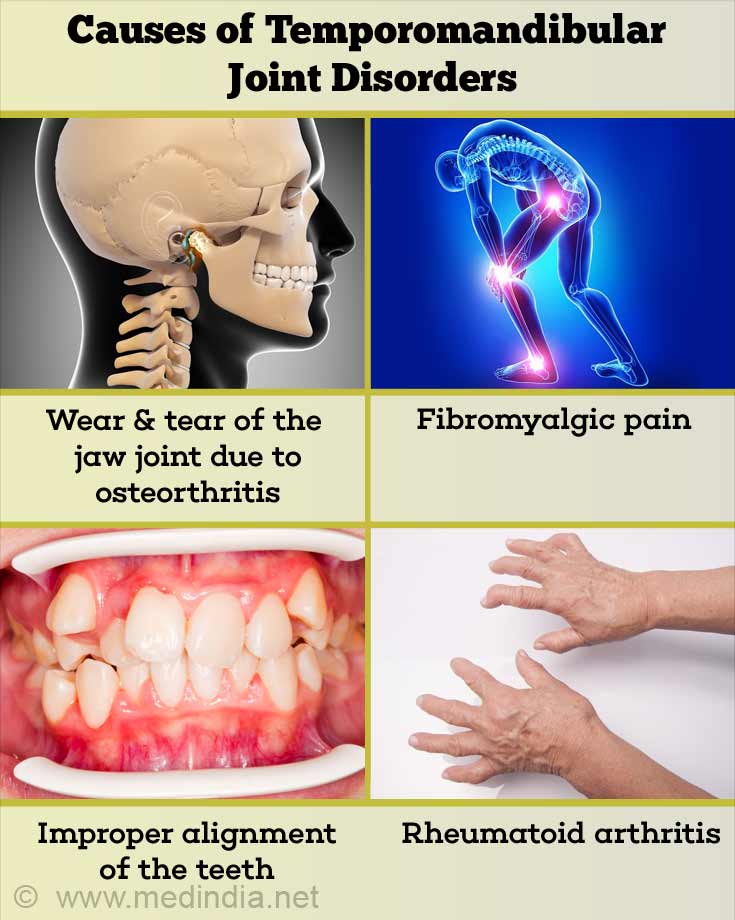
What are the Causes of Temporomandibular Joint Disorders?
In many cases, the exact cause of the TMJ disorder is not known. TMJ disorders are thought to occur due to a complex interplay of multiple poorly understood factors.
Possible causes of TMJ disorder include the following:
- Wear and tear of the jaw joint due to osteoarthritis
- Other joint diseases like rheumatoid arthritis and gout
- Fibromyalgia, which is a chronic disorder causing pain in many joints and muscles in the body
- Trauma to the jaw joint for example, after a blow to the face or surgery
- Increased sensitivity to pain
- Uneven bite or improper alignment of the teeth
- Teeth grinding due to stress
- Displacement of the disc within the joint
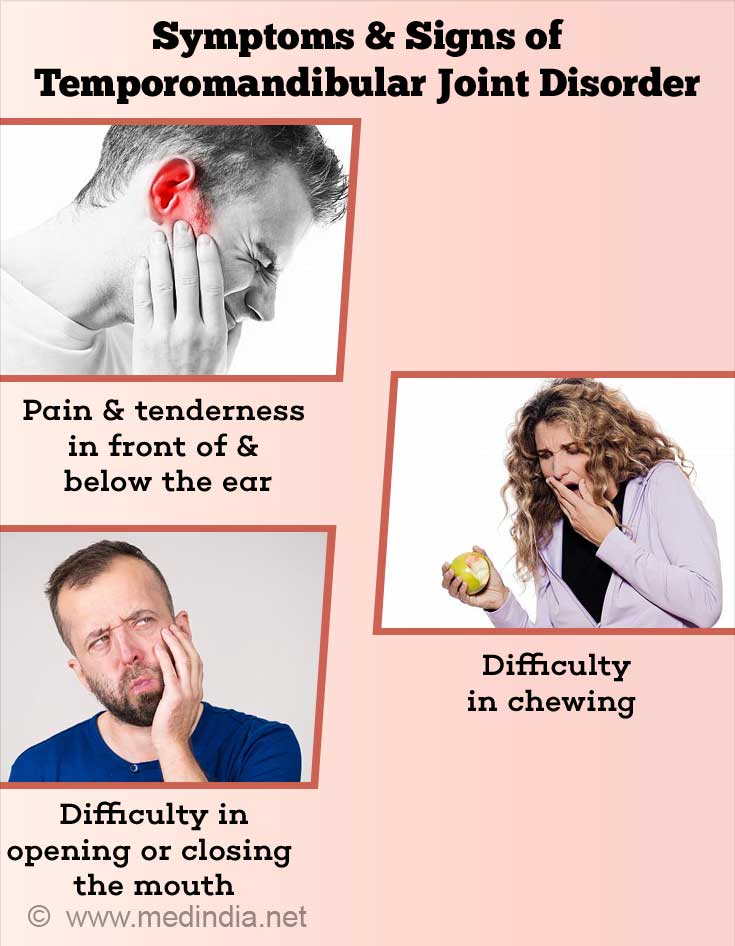
What are the Symptoms and Signs of TMJ Disorder?
A TMJ disorder can cause the following symptoms and signs:
- Pain and tenderness in front of and below the ear, which may spread to surrounding areas
- Difficulty and pain with opening the mouth, chewing food and talking
- Locking of the joint, making it difficult to open or close the mouth
- Clicking or a grating sensation when moving the jaw
How do you Diagnose Temporomandibular Joint Disorders?
TMJ joint disorders are diagnosed by obtaining a detailed medical history from the patient followed by a thorough physical examination and diagnostic imaging if required to confirm the diagnosis or rule out other diseases that may cause similar symptoms.
A Medical History and Physical Examination is necessary to determine the presence of problems in the mouth such as caries, or gum disease. Chronic infection of the sinuses (sinusitis), salivary gland disease and ear infection have to be ruled out before the diagnosis of a TMJ disorder can be made.
The doctor will also test the movements at the joint by asking the patient to open and close the mouth, and check if there is any misalignment of the teeth or problems in the facial muscles.
Diagnostic imaging – An x-ray of the jaw and the teeth, CT scan and MRI imaging may be requested to look for degenerative changes in the joint, problems in the teeth or any other disorder.
Blood tests may be requested if conditions like rheumatoid arthritis or gout are suspected.
How Do You Treat Temporomandibular Joint Disorders?
If the TMJ disorder is a minor problem, which is usually the case, physiotherapy exercises to the temporomandibular joint and lifestyle changes are prescribed.
Lifestyle measures and Exercises
- Avoid opening the mouth too wide
- Eat soft and mashed food till the joint regains strength
- Avoid chewing gum
- Massage the muscles of the face around the joint
- Hold moist heat or an ice pack over the jaw for 10-20 minutes, several times a day
- Do gentle exercises to the jaw muscles as prescribed by the doctor or physiotherapist
- Avoid clenching the teeth
- Avoid resting your chin on your hand
- Adopt stress-relieving measures and relaxation techniques
A mouth guard may be prescribed that fits over the teeth of the patient to prevent damage to the teeth due to grinding at night

Other dental procedures include fitting a crown, bridges or braces, and replacing missing teeth to correct misalignment or a bite problem.
Painkillers such as acetaminophen or other NSAIDs may be prescribed for the symptomatic relief of pain. In case of severe pain, a muscle relaxant, an antidepressant or an opioid analgesic may be prescribed.
Other measures to relieve pain include transcutaneous electrical nerve stimulation (TENS), radio wave therapy, injection of pain-relieving medication into tender muscles of the face called trigger-point injections or deep heat application with ultrasound.
For osteoarthritis of the jaw, steroid injection into the joint may be beneficial in controlling the pain and inflammation. Many patients report improvement within a day or two.
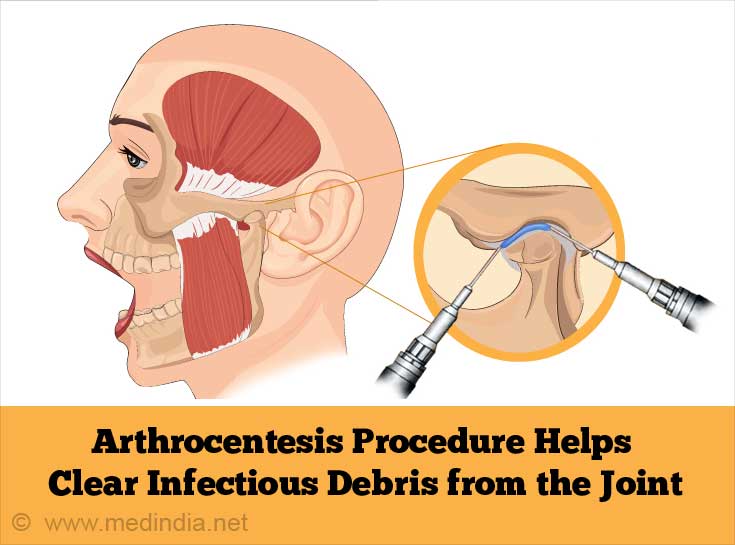
Surgical treatment:
In cases that do not respond to non-surgical conservative forms of treatment, surgery may be recommended. These include the following:
- Joint wash out or arthrocentesis – to clear inflammatory or infectious debris from the joint. This is a minimally invasive procedure that can be done on an outpatient basis.
- Arthroscopy – The doctor views the interior of the joint with a thin illuminated tube and may perform minor corrections or clearing of inflammatory debris. This procedure is relatively less invasive with a smaller scar and a quicker recovery as compared to an open joint surgery.
- Open joint surgery – Open surgery is recommended in cases in which conservative measures do not offer relief and less invasive surgical options are not possible. These may include a tumor affecting the joint, severe degenerative changes with destruction of the joint, or if the joint is filled with bone chips and inflammatory debris.
- The procedure has to be performed by a skilled oro-maxillofacial surgeon and it is advisable to get a second opinion before going in for the surgery. The outlook following open joint surgery is not always good and the surgery has to be undertaken with caution after weighing the pros and cons.