- Hyperparathyroidism - (http://familydoctor.org/familydoctor/en/diseases-conditions/hyperparathyroidism.printerview.all.html)
- Primary hyperparathyroidism - (https://en.wikipedia.org/wiki/primary_hyperparathyroidism#signs_and_symptoms)
- Know About Hyperparathyroidism - (http://www.mountsinai.org/patient-care/health-library/diseases-and-conditions/hyperparathyroidism)
- What is hyperparathyroidism? - (http://my.clevelandclinic.org/health/diseases_conditions/hic_hyperparathyroidism)
- Definition - Hyperparathyroidism - (http://www.mayoclinic.org/diseases-conditions/hyperparathyroidism/basics/definition/con-20022086)
What is Hyperparathyroidism?
Hyperparathyroidism is an endocrine disorder caused by excess amounts of circulating parathyroid hormone (PTH) in the blood. It occurs due to hyperactivity of at least one of the four parathyroid glands in the neck.
The glands secrete excess amount of parathyroid hormone inappropriately, leading to increased levels of calcium in the blood, termed hypercalcemia.
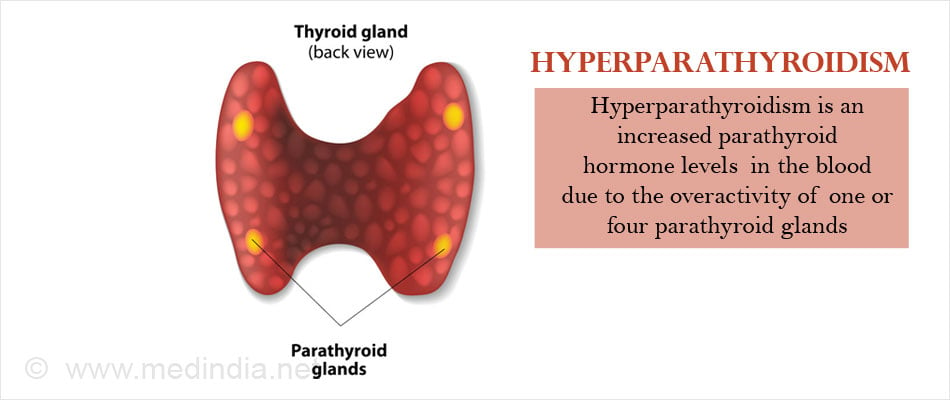
Structure and Function of the Parathyroid Glands
The parathyroid glands, four in number, are situated in the neck behind the thyroid gland. Though their name sounds similar to the thyroid gland due to their location, they are distinct entities, and have a different function.
The upper pair is referred to as the superior parathyroid glands, and the glands situated below are termed inferior parathyroid glands.
Each of the four parathyroid glands resembles a grain of rice and is the color of mustard. The main function of the parathyroid glands is to regulate the blood calcium levels within a very narrow range, which is critical for normal day-to-day functioning.
Role of Calcium in Humans
Calcium is an essential micronutrient which performs three major functions.
- Conduction of electrical impulses by the nervous system - Calcium plays a role in the conduction of electrical impulses along the nerves. This explains why parathyroid disease produces symptoms related to the nervous system, such as weakness, and depression.
- Muscle contraction – Calcium levels within muscles regulate their contraction and relaxation. Parathyroid disease causes muscle weakness and cramps.
- Keeping the skeletal system strong and healthy – Maintaining correct calcium levels is essential for bone health.
How Do Parathyroid Glands Regulate Blood Calcium Levels?
It may be interesting to know that calcium is the only mineral with its own regulatory system, which includes the parathyroid glands.
The parathyroid glands measure the blood calcium levels constantly. Simply stated, if the calcium levels in blood decrease, the parathyroid glands recognize it, and synthesize parathyroid hormone. The PTH makes a suitable withdrawal of calcium from the bones and increases calcium reabsorption from the kidneys and the absorption from the intestines, and replenishes the blood calcium levels. It also causes loss of phosphates through the urine.
Types of Hyperparathyroidism
Types of hyperparathyroidism include the following:
- Primary hyperparathyroidism – Primary hyperparathyroidism occurs due to a pathology in the parathyroid glands. Surgery on the glands can help treat hyperparathyroidism.
- Secondary hyperparathyroidism – Secondary hyperparathyroidism occurs due to the presence of kidney failure, which causes low calcium levels. Over time, the parathyroid glands respond by secreting more parathyroid hormone to try and maintain blood calcium levels within normal limits.
There is another entity referred to as tertiary hyperparathyroidism. Here, the parathyroid glands which have until then been stimulated by low calcium levels in diseases such as kidney failure, begin to function autonomously (unregulated), due to persistent stimulation. Treatment remains the same as that for secondary hyperparathyroidism.
What are the Causes of Hyperparathyroidism?
- Primary hyperparathyroidism – The causes of primary hyperparathyroidism include:
- Parathyroid adenoma – Parathyroid adenoma is a benign non-cancerous growth of a parathyroid gland. It is the most common cause for primary hyperparathyroidism.
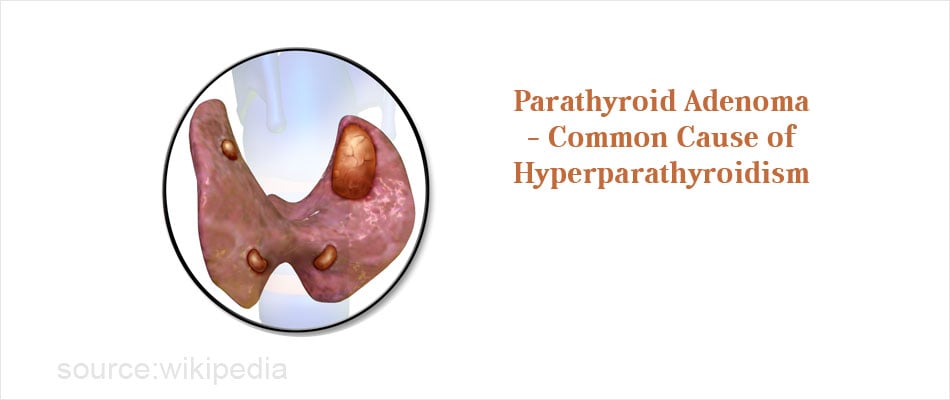
- Parathyroid hyperplasia – Parathyroid hyperplasia is a condition where the parathyroid glands are enlarged.
- Parathyroid cancer – Parathyroid cancer is a rare cause of primary hyperparathyroidism. It is a malignant (cancerous) growth involving the parathyroid gland.
Majority of cases of primary hyperparathyroidism (95%) occur sporadically, but a small minority (5%) are familial associated with genetic mutations.
An example of a genetic condition associated with parathyroid tumors (leading to hyperparathyroidism) is Multiple Endocrine Neoplasia I (MEN I) syndrome. In this condition, a genetic mutation predisposes to multiple endocrine tumors including tumors of the parathyroid.
- Secondary hyperparathyroidism – Secondary hyperparathyroidism occurs due to an underlying condition that decreases serum calcium levels. Causes of secondary hyperparathyroidism include
- Chronic kidney failure – It is the most common reason for secondary hyperparathyroidism. In kidney failure, the body is unable to convert vitamin D to its active form namely calcitriol. Reduced calcitriol level results in lowered calcium levels in the blood.
- Stomach bypass surgery for obesity – Stomach bypass surgery reduces the surface area for absorption of calcium from the food, leading to calcium deficiency.
- Celiac disease – Celiac disease is a disease of the small intestine causing malabsorption of various nutrients including calcium.
- Crohn’s disease – Crohn’s disease is an inflammatory bowel disease affecting the small intestine, and is associated with malabsorption of nutrients, leading to various deficiencies.
- Severe vitamin D deficiency - Vitamin D helps to maintain calcium levels of blood by promoting intestinal absorption of calcium. In vitamin D deficiency, either due to dietary lack or as a result of malabsorption, calcium levels in blood may decrease, which stimulates the parathyroid to secrete more hormone.
What are the Risk Factors for Hyperparathyroidism?
Risk factors for hyperparathyroidism include the following:
- Post-menopausal women
- Multiple Endocrine Neoplasia Type I – a rare genetic condition affecting multiple endocrine glands, and associated with a higher incidence of primary hyperparathyroidism
- Other genetic disorders like hyperparathyroid-jaw tumor (HPT-JT) syndrome, and familial isolated hyperparathyroidism (FIHPT) also increase the risk of primary hyperparathyroidism
- History of neck irradiation
- Taking lithium – a drug used in the treatment of bipolar disorder
What are the Symptoms and Signs of Hyperparathyroidism?
Symptoms of primary hyperparathyroidism are caused by hypercalcemia. They are classically referred to in the following terms, namely "stones, abdominal groans, bones, thrones and psychiatric overtones".
- "Stones" mean kidney stones. The patient may also suffer from increased urination and thirst due to diabetes insipidus. The patient may ultimately suffer from kidney failure.
- "Abdominal groans" include gastrointestinal symptoms such as nausea and vomiting, constipation, and indigestion. Hypercalcemia can cause peptic ulcers and acute inflammation of the pancreas (pancreatitis). The cause of peptic ulcers in hyperparathyroidism is suggested to be the increased gastric acid secretion that occurs in hypercalcemia.
- "Bones" refer to complications occurring in the bone, which include osteoporosis, arthritis, osteomalacia and rarely osteitis fibrosa cystica. The patient may complain of bony pain and occasionally even pathological fractures.
- "Thrones" refer to the constipation and polyuria that occurs in hypercalcemia.
- "Psychiatric overtones" allude to the effects on the nervous system. Symptoms include tiredness and lethargy, depression, distorted sense of reality (psychosis), unsteady movements (ataxia), confusion, delirium, and occasionally coma.
In addition, the patient may also suffer from cardiovascular conditions like hypertension and reduced heart rate.
- Secondary hyperparathyroidism also produces similar symptoms which may include:Bone deformities
- Fractures
- Swelling of joints
Other features relating to the underlying cause of secondary hyperparathyroidism like kidney failure, malabsorption syndromes and rickets can occur.
Some patients may develop a condition referred to as calciphylaxis where deposits of calcium occur in the skin and muscles leading to painful lesions in the skin that may ultimately break down and ulcerate.
How is Hyperparathyroidism Diagnosed?
It is important to distinguish between primary and secondary hyperparathyroidism, since the treatment is very different.
Primary Hyperparathyroidism
1. Blood tests
The disease is typically diagnosed by blood tests. The characteristic findings include:
- Elevated levels of calcium in the blood (hypercalcemia) associated with elevated levels of parathyroid hormone. Normal calcium levels are 2.2 to 2.7 mmol/L.

2. Diagnostic imaging
Once a diagnosis of primary hyperparathyroidism is established, imaging tests are done to localize the lesion in the parathyroid gland.
- Ultrasonography is an useful diagnostic imaging test to localize suspicious parathyroid lesions.
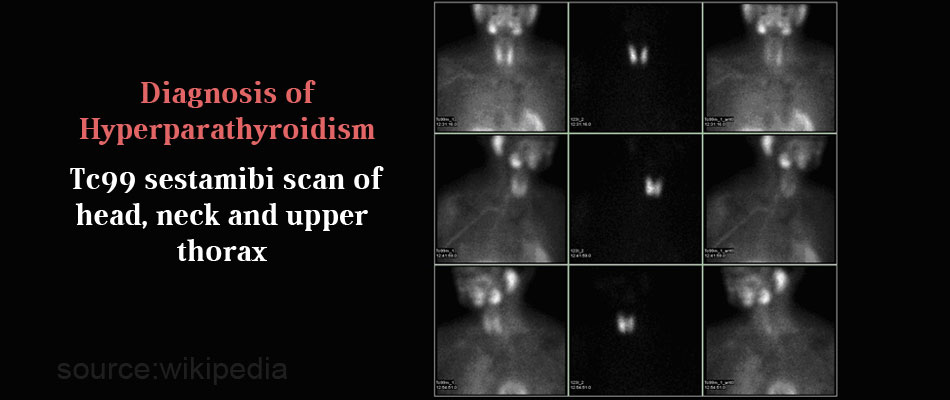
- Tc99 sestamibi scan of head, neck and upper thorax is the diagnostic test most often employed to localize parathyroid adenomas. It has a sensitivity and specificity of 70-80%. Sestamibi is a radioactive substance, absorbed by parathyroid gland that are hyperactive, and can be recognized by a scanner which detects radioactivity.
Secondary Hyperparathyroidism
1. Blood tests – The characteristic findings are:
- Low serum calcium levels (hypocalcemia) and elevated PTH levels
- Phosphorus levels will be low if there is malabsorption, or high in cases of kidney failure
- Vitamin D3 levels may be low in kidney disease

2. Bone x-rays and bone density scans
Bone x-rays and bone density scans will help to diagnose fractures, bone thinning and bone loss, and softening of bone.
Tests to detect the underlying condition like kidney function tests and ultrasound of the kidneys should also be done.
How is Hyperparathyroidism Treated?
Watchful approach
In both primary as well as secondary hyperparathyroidism, the physician may adopt an approach of watchful waiting under the following circumstances.
- Serum calcium levels are only mildly increased
- Kidney function is normal, and there is no evidence of kidney stones
- Bone density is normal or only minimally reduced
- No other troubling symptoms
In such cases, regular monitoring of serum calcium, bone density and kidney function is critical.
1. Primary Hyperparathyroidism
Surgery
Surgery is the mainstay in the management of primary hyperparathyroidism. Parathyroidectomy should be performed only by skilful surgeons experienced in the procedure. Indications for surgery include patients who are symptomatic or in asymptomatic patients, if they satisfy any ONE of the following criteria.
- Serum calcium levels 1.0 mg/dL (0.25 mmol/L) or higher than the upper limit of normal
- Reduced kidney function with a creatinine clearance <60 mL/min
- Osteoporosis with bone density at the hip, distal radius or lumbar spine less than peak bone mass by more than 2 standard deviations (T score <-2.5)
- History of prior fragility fracture
- Age less than 50 years of age
Medications
Drugs used to treat primary hyperparathyroidism include the following
Calcimimetics
Calcimimetics are a group of drugs that mimic the action of calcium circulating in the blood.
Cinacalcet is a calcimimetic that has been primarily approved for treatment of hyperparathyroidism due to chronic kidney disease or parathyroid cancer. However, some doctors may give this drug for other causes of primary hyperparathyroidism, if

- The patient is not a suitable candidate for operation
- Surgery is not likely to be curative
2. Secondary Hyperparathyroidism
In secondary hyperparathyroidism, the treatment of the underlying cause of low calcium levels in blood (hypocalcemia), may be curative.
- Patients with chronic renal failure are advised calcium and vitamin D3 supplements, and restriction of phosphate in their diet. Phosphate binders like sevelamer hydrochloride or lanthanum carbonate may be given if necessary.
Cinacalcet (Sensipar), a calcimimetic may also be given. The drug may trick the parathyroid glands to decrease the release of parathyroid hormone.
Dialysis, renal (kidney) transplant, or in certain cases, parathyroid surgery may become necessary.
- Patients with malabsorption syndromes, or those who have undergone weight loss surgery are advised calcium and vitamin D3 supplements.
In post-menopausal women, hormone replacement therapy may reduce calcium loss from bone and address the symptoms of osteoporosis.
Biphosphonates may also be given to address osteoporosis, and lessen loss of calcium from bones in hyperparathyroidism.
How Can Hyperparathyroidism be Prevented?
- In familial cases of primary hyperparathyroidism, the family members should be advised to undergo regular monitoring of blood calcium levels to check for hypercalcemia (increased calcium levels)
- Adequate calcium and vitamin D supplements may prevent secondary hyperparathyroidism in women
- Persons with kidney disease, or malabsorption syndromes should also take regular calcium and vitamin D3 supplements.
Health Tips
- Post-menopausal women should take adequate supplements of calcium and vitamin D to prevent secondary hyperparathyroidism.
- Persons with chronic kidney disease, malabsorption syndromes and vitamin D deficiency should take regular supplements of the same.
- In rare cases of familial primary hyperparathyroidism, first degree relatives should be regularly monitored for calcium levels.






