- Cystocele (Prolapsed Bladder) - (https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems-women/cystocele-prolapsed-bladder)
- Vaginal Repair of Cystocele with Anterior Wall Mesh via Transobturator Route: Efficacy and Complications with Up to 3-Year Followup - (http://dx.doi.org/10.1155/2009/743831)
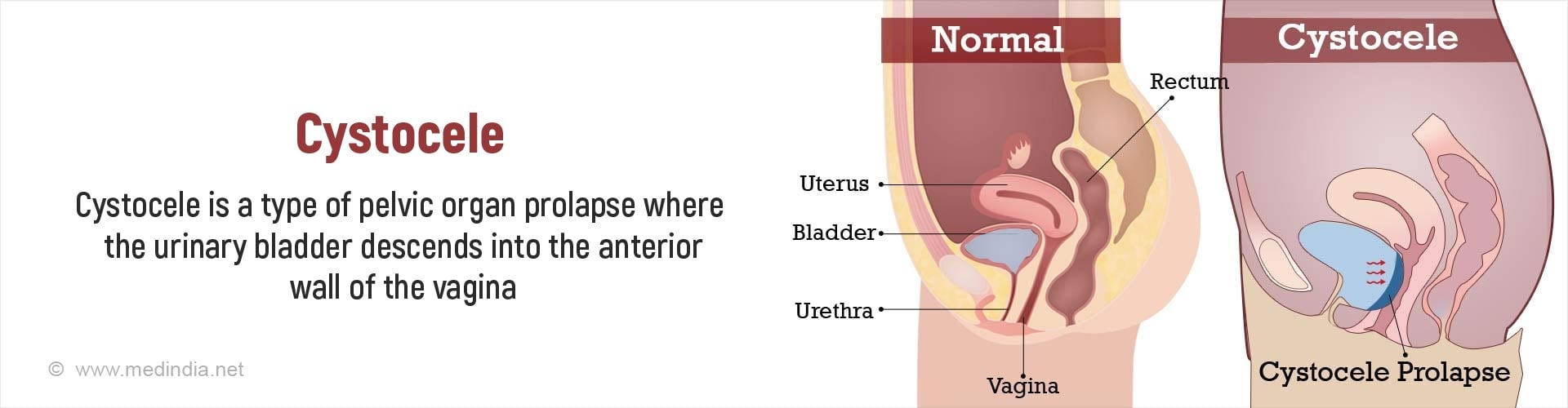
What is Cystocele?
Cystocele is a type of pelvic organ prolapse where the urinary bladder moves downward along the anterior vaginal wall and towards the vaginal opening in females. It occurs due to the lack of support to the urinary bladder from tissues between the bladder and the vagina. The prolapse of the urethra along with the urinary bladder is called cystourethrocele.
Relevant anatomy of the pelvic region: The pelvis is the part of the trunk below the abdomen that is enclosed in a bony bowl-shaped structure consisting of the hip bones and the lower spine. It contains organs associated with reproduction as well as the lower part of the digestive tract, the rectum. The pelvic floor separates the pelvis from the perineum and consists of muscles and other tissues that support the urinary bladder and the rectum, and the vagina in females. The perineum in obstetrics and gynecology is the area including the anus and in females, the vagina. The pelvic floor has two openings, the urogenital hiatus in front (which allows the passage of the urethra and the vagina in females) or the urethra in males, and the anal hiatus behind that allows the passage of the anus.
The urinary bladder is located in the front of the pelvic region with the uterus in females located over and above it. The outlet of the uterus, the cervix, opens into the vagina which passes behind the urinary bladder and through the urogenital outlet to open out in the perineum.
What are the Causes of Cystocele?
Cystocele occurs due to lack of support to the urinary bladder because of the weakening of the tissues between the bladder and the vagina. As a result, the bladder bulges into the anterior vaginal wall. The weakness may occur due to genital atrophy following aging or multiple pregnancies.
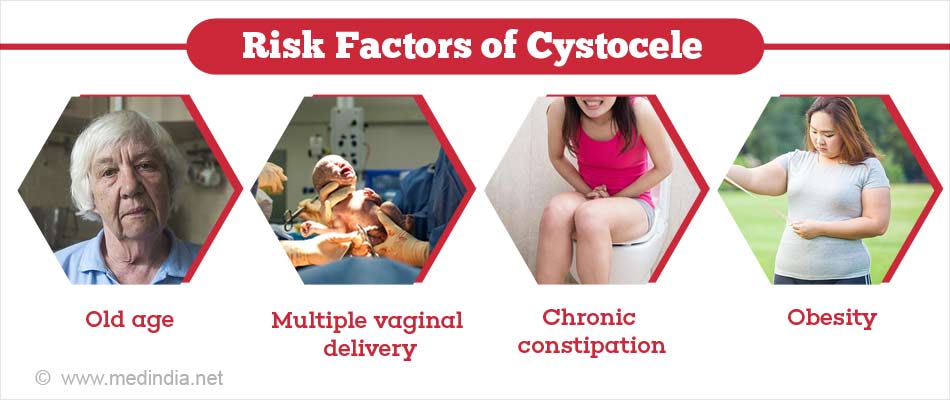
What are the Risk Factors of Cystocele?
The risk factors for cystocele include the following:
- Older age, due to age-related damage to the muscles and other tissues
- Higher number of vaginal deliveries, which weaken the pelvic muscles
- Presence of a family history of cystocele
- Hormonal deficiency
- Obesity
- Conditions that increase the pelvic pressure and weaken the pelvic floor. These include chronic cough, straining while passing stools due to chronic constipation, or lifting heavy weights
What are the Symptoms and Signs of Cystocele?
Mild cystoceles may not cause any symptoms. The symptoms and signs of moderate-to-severe cystoceles may include the following:
- A feeling of pressure in the pelvic region, or a feeling that something is falling off the vagina
- Difficulty in emptying the urinary bladder completely
- Increased urinary frequency and urgency to pass urine due to incomplete emptying of the bladder. The incomplete emptying of the bladder also promotes infection in the residual urine
- Urinary incontinence in conditions that increase pressure on the bladder like coughing or walking

How do you Diagnose Cystocele?
Cystocele is diagnosed based on the following:
- History obtained from the patient, who may complain of some of the above-mentioned symptoms
- Physical examination. The diagnosis of cystocele can often be made on the basis of a physical examination alone. During a vaginal examination, the doctor will be able to feel the urinary bladder bulging through the anterior wall of the vagina; the bulging becomes more pronounced when the patient coughs. The doctor will also grade the cystocele from grades 1 to 3 depending on the extent of the bulge; grade 1 is when there is a mild drop of the bladder into the vagina. In grade 2, the bladder reaches the opening of the vagina. Grade 3 is the most severe form with the bladder bulging out of the opening of the vagina.
- Diagnostic tests. Tests are carried out to understand the degree of urinary retention and post-void residual urine in the bladder after passing urine. These include:
- Ultrasound, where a probe is passed over the lower abdomen to assess the amount of urine in the bladder.
- Catheterization of the bladder, where a tube is passed into the bladder along with aseptic precautions to drain the urine from the bladder. A local anesthetic may be applied to avoid discomfort during the procedure.
Both the above tests are repeated after the patient passes urine to measure the post-void residual urine.
- Voiding cystourethrogram, in which a contrast dye is inserted into the urinary bladder through a catheter and x-ray images are obtained while the patient passes urine. The test is used to study how the bladder is affected by the cystocele.
How do you Treat Cystocele?
Cystocele is treated with the following:
- Kegel exercise: Kegel exercises are simple exercises to improve the strength of the pelvic muscles that a woman can do comfortably at home. The bladder should be emptied before doing the exercises and the patient should be instructed the following:
- The pelvic floor muscles should be contracted for a period of 5 to 10 seconds. These are the muscles that, when contracted, can stop the flow of urine midway. The person should breath normally and should not contract any other muscles at the same time to avoid pressure on the urinary bladder.
- The contraction should be followed by relaxation of the muscles for a similar duration.
- The contraction and relaxation should be repeated around 10 times in each session, with the sessions being repeated around three times in the day. The exercises should be ideally done in the lying down, sitting and standing positions.

- Insertion of a pessary into the vagina: Vaginal pessaries are plastic or rubber rings that provide support to the urinary bladder and can be inserted through the vaginal opening. The pessary should be changed every 6 months. It could be used in women with cystocele who cannot undergo or do not wish to undergo a surgery.
- Surgery is used for the treatment of cystoceles that gives rise to symptoms.
- Anterior colporrhaphy. In this procedure, an incision is made through the anterior wall of the vagina and the tissues between the bladder and urethra on one side, and the vagina are tightened to provide added support to the bladder. The procedure can give rise to complications like shortening and narrowing of the vagina. The use of a mesh to support the bladder often has better outcomes and reduces the chances of recurrence of the cystocele. However, it is associated with complications which may include extrusion of the mesh, pain in the vagina or surrounding areas, pain during sex, infection or fistula formation. Antibiotics are prescribed to prevent infections due to the procedure. The local application of estrogen before the surgery may also help to improve the outcome.
- Paravaginal repair: This procedure is used less often. It is carried out either through an abdominal or vaginal approach.
How do you Prevent Cystocele?
Steps that can be taken to prevent a cystocele include the following:
- Kegel exercises can be performed even by healthy individuals to improve the strength of the pelvic musculature and prevent the development of a cystocele
- Conditions that predispose to cystocele like chronic cough and constipation should be treated early
- Family planning methods should be adopted to reduce the stress on the pelvic tissues caused by repeated vaginal deliveries
- Weight reduction should be attempted by obese individuals