A recent study published in the November issue of the Journal of the National Cancer Institute, shows that paternity rates of testicular cancer patients declined after treatment, and patients treated with the higher chemotherapy dose had the lowest chance of becoming fathers.
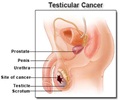
Germ-cell testicular cancer is the most common cancer among 20-40 year old men. Many testicular cancer patients are diagnosed at an age at which they are starting a family, and the ability to father children in the future is an important issue for approximately 60% of newly diagnosed patients.Subfertility or infertility can be associated with the disease itself or with its treatment. Approximately half of all testicular cancer patients have defective spermatogenesis at diagnosis, even before orchiectomy.
Researchers from Norway assessed post-treatment paternity among long-term survivors of testicular cancer whose treatment had followed a modern management approach. A total of 1814 men who had been treated for unilateral testicular cancer in Norway during 1980 through 1994 were invited to participate in a national multi-center follow-up survey in 1998 through 2002.
The participants were allocated to five groups according to the treatment received after orchiectomy, including treatment at relapse (surveillance, retroperitoneal lymph node dissection, radiotherapy, low-dose chemotherapy, and high-dose chemotherapy).
Results obtained depicted that a total of 1433 men were assessable, of whom 827 were fathers at diagnosis. 554 men had attempted post-treatment conception, among whom the overall 15-year actuarial post-treatment paternity rate was 71% without the use of cryopreserved semen. This rate ranged from 48% in the high-dose chemotherapy group to 92% in the surveillance group.
Assisted reproductive technologies were used by 22% of the couples who attempted conception after treatment. Dry ejaculation, treatment group, pretreatment fatherhood, and marital status were statistically significant independent predictors for post-treatment fatherhood, with dry ejaculation as the most important negative factor.
Advertisement
Although the overall paternity rate after treatment for testicular cancer was high, the ability to conceive and the time to conception reflected the intensity of treatment. The authors hope that these data may help inform patients about their future ability to father biological children