‘Estrogen therapy helps to reduce some of the risk in women who have undergone ovarian removal.’
Tweet it Now
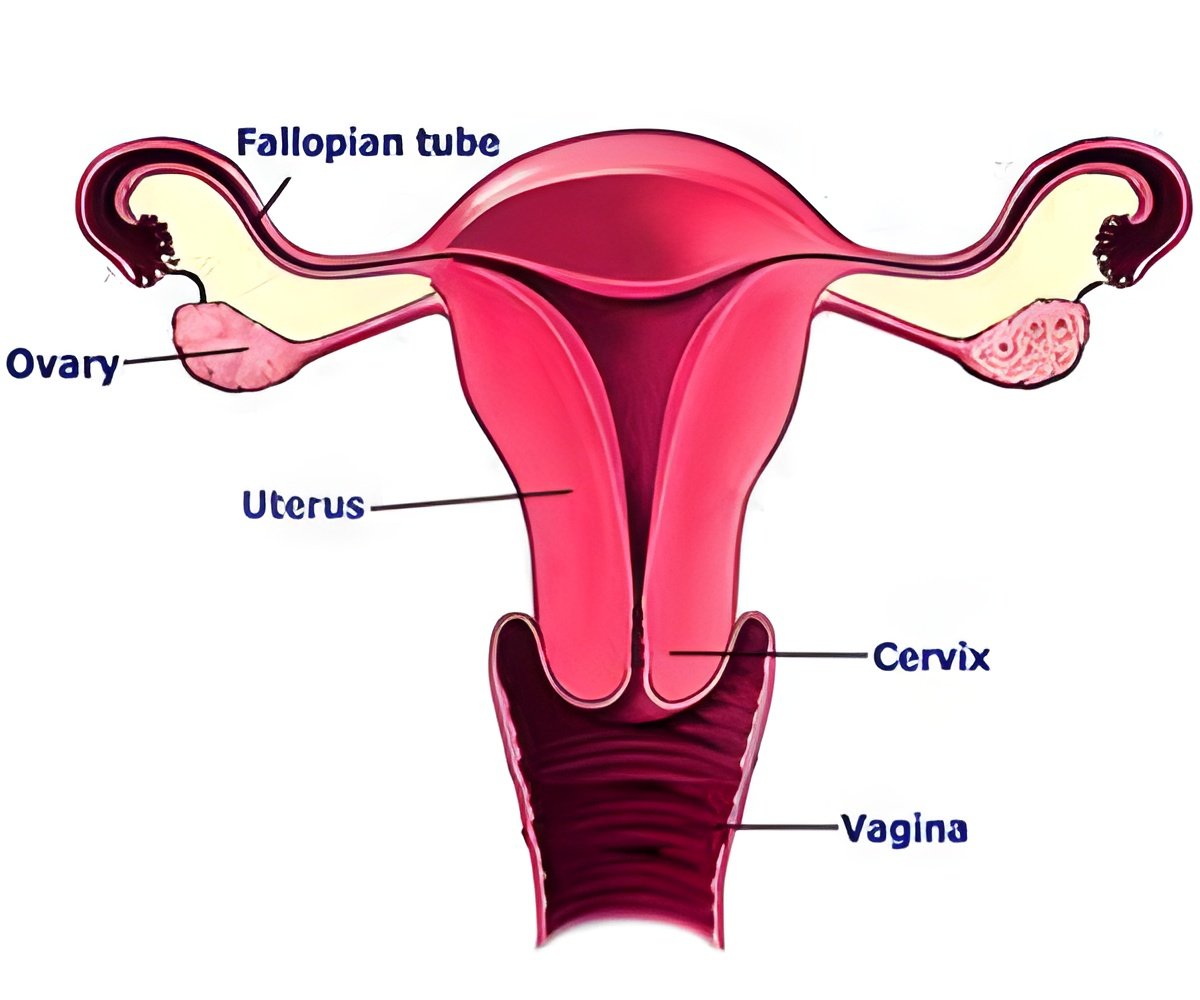
Bilateral oophorectomy is the formal term for removal of both ovaries, often used as a preventive measure against ovarian cancer. For the first time, the team of nine researchers from multiple disciplines linked bilateral oophorectomy to a marked increase in 8 of the 18 chronic health conditions that were measured.The effects of oophorectomy in premenopausal women are much broader and more severe than previously documented.
“This study provides new and stronger evidence against the use of bilateral oophorectomy for prevention in young women,” says Walter Rocca, M.D., lead author of the study. “Bilateral oophorectomy should not be considered an ethically acceptable option for the prevention of ovarian cancer in the majority of women who do not carry a high-risk genetic variant.”
The study, published in the peer-reviewed journal Mayo Clinic Proceedings followed two groups of women for a period of approximately 14 years. There were 1,653 women who underwent bilateral oophorectomy and an equal number of women of the same age who did not. The study was made possible by using the records linkage system of the Rochester Epidemiology Project.
Results showed that women under 46 who underwent bilateral oophorectomy experienced a higher incidence of the 18 chronic conditions considered one at a time, except cancer, and an accelerated rate of accumulation of combined conditions, or multimorbidity.
Advertisement
The investigators suggest that the premature loss of estrogen caused by the oophorectomy may affect a series of aging mechanisms at the cellular and tissue level across the whole body leading to diseases in multiple systems and organs.
Advertisement
Source-Medindia














